Episode 9
Published on Wednesday, November 16, 2016
According to CMS, The Comprehensive Primary Care (CPC) initiative is a four-year, multi-payer initiative designed to strengthen primary care. In our latest podcast, Dr. Randy Walker and Angie Walker, from Dr. Randy Walker Family Practice & Allergy Clinic, outline their experience with CPC and how they joined the program.
“Dr. Walker created a risk stratification tool before we started CPC. That tool was based on disease, where you’re at in your disease, and your utilization in services. So when we came into eCW, we were able to create that tool into the note, so that when the nurses pull those patients back, they automatically risk stratify them every time.”
Angie Walker – Office Manager, Walker Family Practice

Topics from this episode
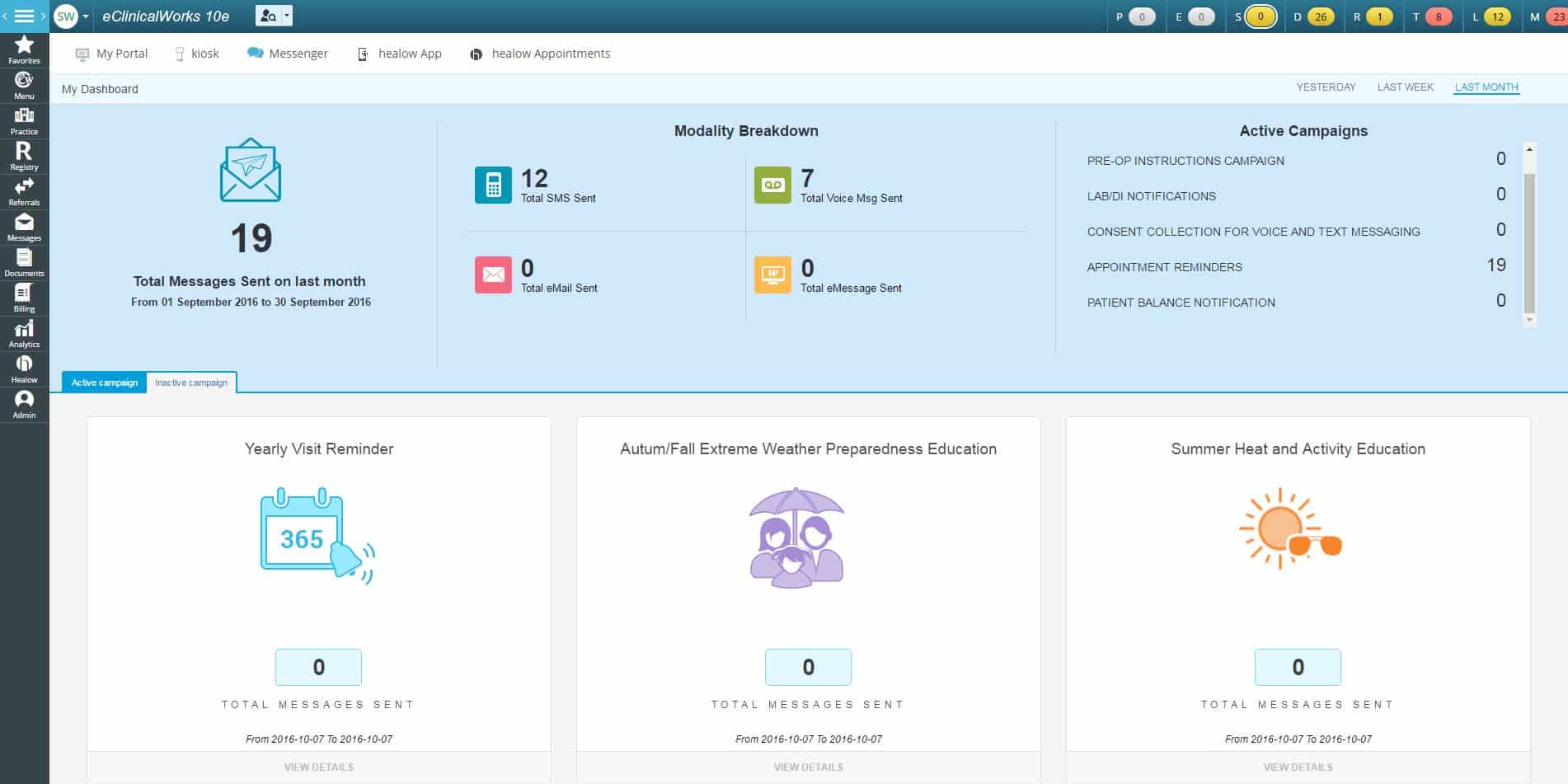
eClinicalMessenger dashboard
The eClinicalMessenger dashboard allows practices to track the effectiveness of their Messenger campaigns, including how well there are reaching targeted audiences for health reminders. Improved outreach means enhanced patient care and higher patient satisfaction. The dashboard helps practices determine whether they are on track to realizing increased office efficiency, streamlined workflows, and best use of staff resources.
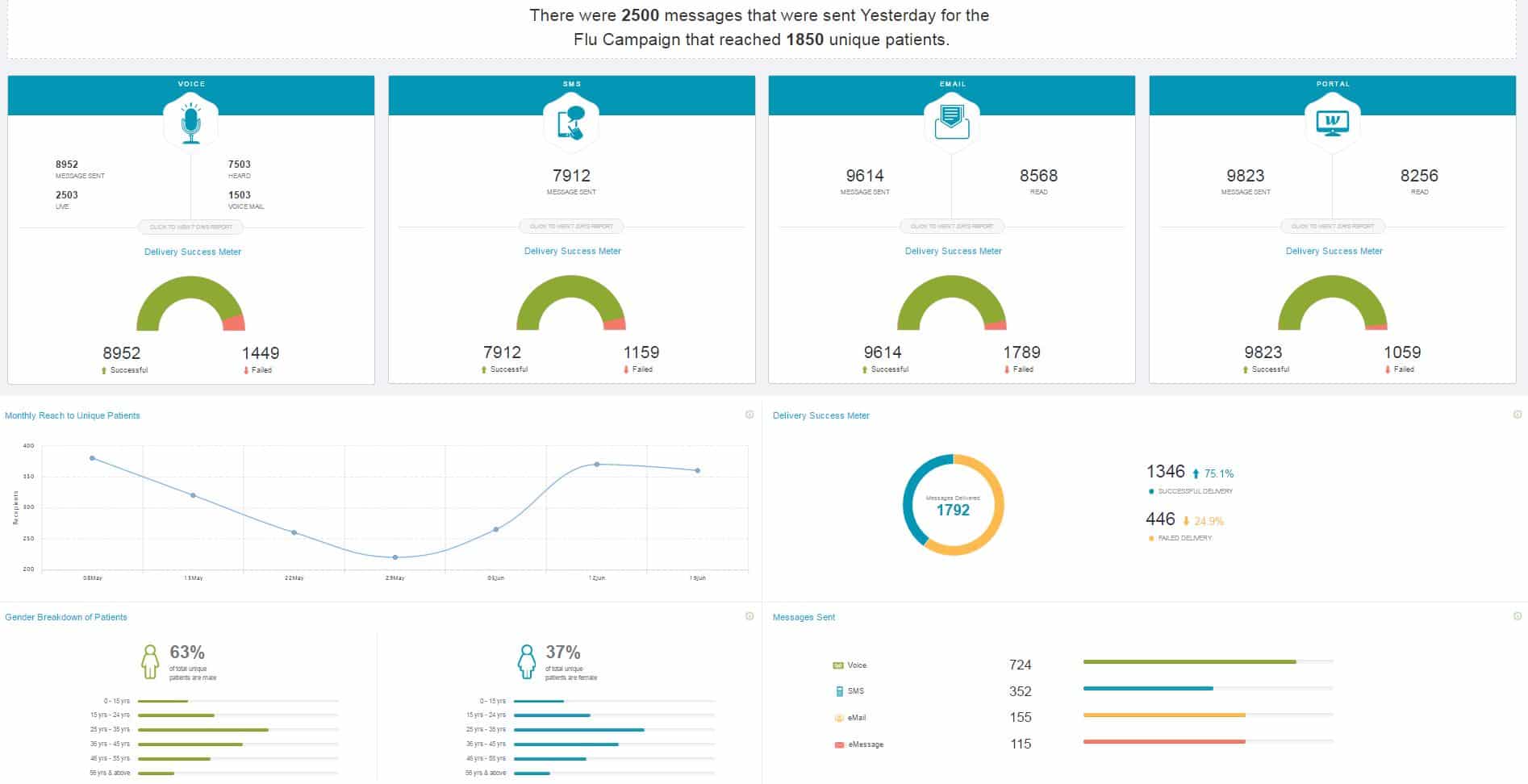
Flu campaigns dashboard
The flu campaign dashboard is an example of how healthcare IT technology can gauge the effectiveness of a practice’s outreach efforts on a simple yet vital wellness effort — annual flu campaigns. The dashboard details the number of messages sent, and the method of delivery, whether by voice, email, SMS, or eMessage. Providers can also see the overall and gender-specific delivery success rates.
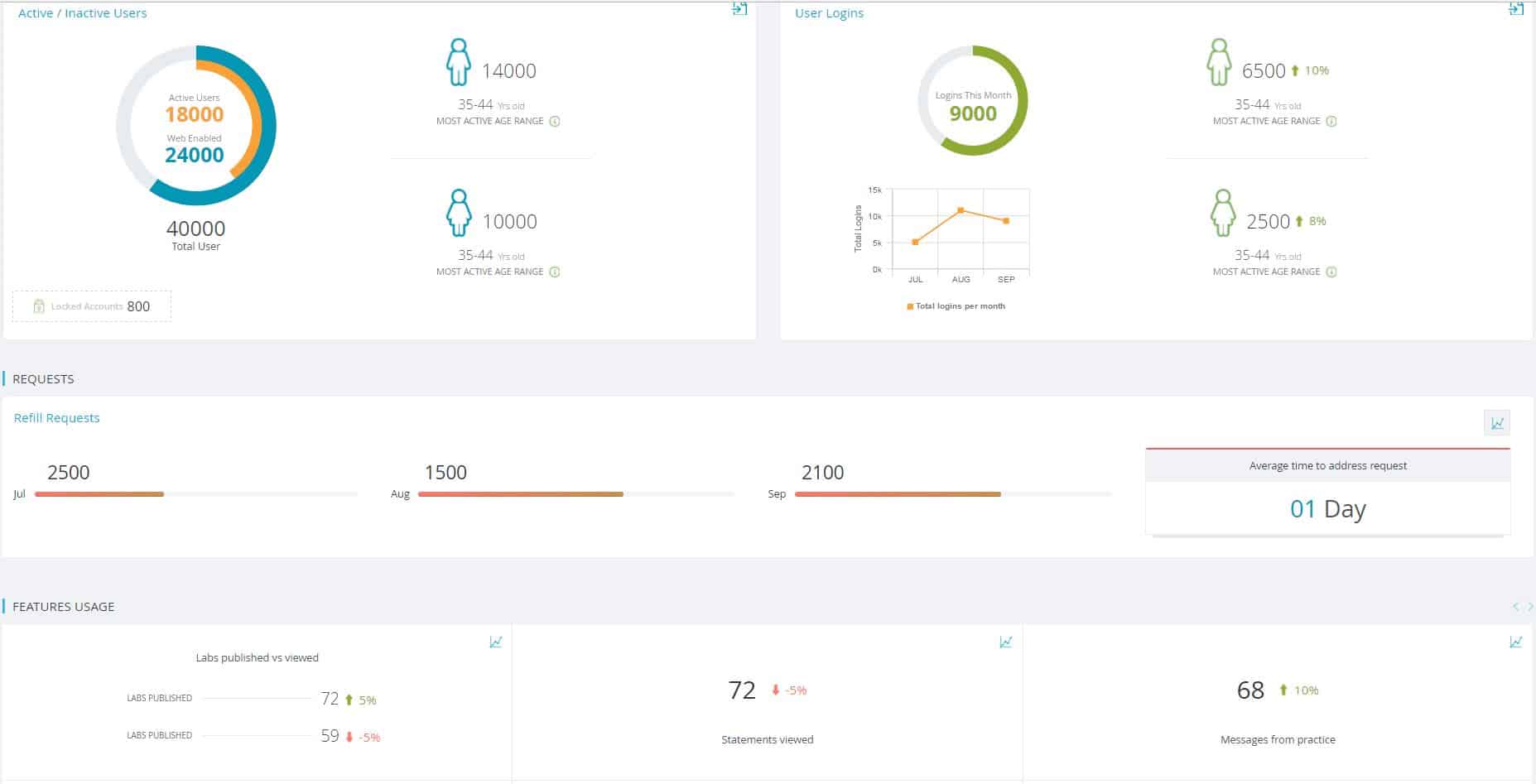
Patient Portal dashboard
The eClinicalWorks Patient Portal is a leading tool for medical practices, empowering patients to be fully engaged in their own healthcare, with access to medical records, appointments, labs, and secure messaging. For practices, the Patient Portal dashboard summarizes patients’ clinical data for reporting purposes under the CPC. Practices can gauge the effectiveness of patient engagement efforts, track compliance, and transfer data into reporting modules.
Brian: Welcome to another eCW Podcast, I’m your host, Brian Saal, and we’re here in De Queen, Arkansas, speaking with Dr. Randy Walker and Angie Walker. Today’s topic is going to be Comprehensive Primary Care Initiatives, CPCI. First of all, thank you so much for being with us today, we really appreciate your time. Before we get started with the questions, can you tell us a little bit about your practice to begin with — what sort of population do you see. You’re a family practice, you’ve got some allergy work going on there, as well, but just give us a general sense about what your practice is like.
Randy: Really, we see from birth to death, and we set fractures and EKGs and x-rays, and we really just try to take everything that comes through the door.
Brian: Full suite.
Randy: Full service, yeah.
Angie: I would say we have an active patient population, with a look back of about one to two years, probably about 3,500 to 4,000 active patients.
Brian: That’s fantastic. So let’s start talking about CPCI. How did you first learn about the initiative?
Angie: we work pretty closely with AFMC, which is the Arkansas Foundation for Medical Care. My liaison or my rep, Kim Miller, came into the office one day and said, ‘Hey there’s a really great program that’s coming out, and we think you should apply for it.’ We’re very proactive in programs that are coming down the pike, especially those that are pilot that people are studying and watching because we want to know – we want to be ahead of any changes that are coming. So we had just finished up a program with them and she said, ‘You guys, you would roll right into it, this would be perfect for you.”
Brian: Actually I should take a step back, and if we could give a brief description of what CPCI is. CPCI is a program that was put in place by the Centers for Medicare and Medicaid Innovation in 2012. It’s a four-year program, it’ll be ending at the end of this year, 2016, and will be replaced by CPC Plus. The initiative is to pay selected caregivers, across a certain number of regions of the United States — it’s sort of a pilot program — and then see how well the program is working before launching it to CPC Plus. That’s just a very, very brief overview of it, but I think we’ll be able to get a little more in depth as we talk about it this morning. So when did you actually get involved with CPCI?
Angie: We were in it from the get-go, and so we had just finished up the Arkansas Chronic Illness Collaborative, which was a lot of the same things that CPCI was coming into, so we had just finished that collaborative and found out about CPCI, so we applied for it and got in it. So we started from the get-go.
Brian: Can you tell me a little about the application process? What was that like?
Angie: It’s a very easy process. They needed to know your patient demographics, so you have to be able to identify your active patient population, race, demographics, ethnicity, and things of that nature.
Brian: There’s also a technology component to it, as well.
Angie: Yes, especially in CPC Plus, if you’re moving and you try to, you very much have to have an active relationship with your EMR HIT vendor.
Brian: Now CMS offers, for a lack of a better term, call them incentive programs, such as Chronic Care Management, where if the patient is seen for 20 minutes outside of the office, the office can bill $42 a month. But there are some caveats that go along with that — a patient needs to sign a consent form, and also has to pay an $8 per month copay. Does CPCI have any of those sorts of requirements? Is there consent forms that need to be signed? Or additional payments made?
Angie: No, and for the most part when you do CPCI, you can’t do the Chronic Care Management part of it. With CPCI, we are required to make sure that we have notices in the office that say, ‘We are participating in this project, and if you wish not to participate in it, your data not to be discussed and what have you, you can ask to be removed.’
Brian: Okay so you can opt out of the program if you if you choose, but there’s no opt in, so to speak?
Angie: No, you’re automatically and you have to make an effort to opt out.
Brian: Now one of the unique things about CPCI is its payment model. So, if I understand this correctly and please correct me if I’m wrong, I understand that it will still allow you to bill fee-for-service, but then on top of that there is a monthly, per patient, per month, fee that you’re going to receive, and then there’s also some shared savings. Have you been involved with all of those three areas?
Angie: So, yes, in CPCI, it’s a risk management fee, based on the patient’s risk level that you get to help with those expenditures. Arkansas did not receive shared savings for this previous year. It is a little bit of an alternative payment model there.
Brian: Okay let’s dive a little deeper, and talk a little bit about the five primary care functions, which are the access and Continuity, Planned Care for Chronic Conditions and Preventive Care, Risk-stratified Care Management, Patient and Caregiver Engagement, and coordination of care across the medical neighborhood. Can we go through each one? Can you talk about any struggles that you’ve had or, even better than struggles, would be how you accomplished meeting these guidelines? So, access in continuity…
Angie: So that one I think was a pretty easy one for us, like I said, in the beginning we did not have eCW as our vendor for the first year, and quickly realized that we had to do something different. We wanted something that had better patient engagement because we needed that. And so, when we moved into eCW, we were able to do your access via the Patient Portal, so you have huge access and availability to things on your Portal. As far as the office was concerned, we basically at that point had hired a nurse practitioner, and so we looked at a staggered schedule. Initially we just staggered lunches, so Monday through Friday, took all major holidays and what have you, and as we moved into that second year of the program, it was like OK, if we’re going to give access to patients, we’re going to have to really look at these things. So the nurse practitioner decided that she would like to come in at 7 o’clock in the morning, working until 4 o’clock, and then Dr. Walker decided that he would like to come in at 8:30 and go until at 5:30. So not only did we get two extra hours in the morning, an extra 30 minutes during the day, and we also have these staggered lunches. But then we also had both of them doing urgent access appointments, so for each of them, they had an hour at every day that could not be booked until that day, for those patients that called at that time. And then, as any clinic does, we have standard times that you overbook for no-show. And so we have the same thing going on.
Randy: And then as far as the continuity, when we got eCW, I said, ‘Hey you know this looks like it was written by doctors.’ And, come to find out, it was! As far as the continuity part of that picture goes, it really allows one provider to communicate with another provider very efficiently.
Brian: So, transition of care is that much easier.
Randy: a big part of the medical record is just redundancy, and eCW allows for that, but then there’s certain parts of the medical record that are very important for one provider to be able to efficiently transmit to the next provider, and it does that well.
Brian: Well, I guess the follow-up question to that would be: Have you added any staff once you got into the program, to help accommodate CPCI?
Angie: We’ve retrained staff.
Randy: You know, I would say that we didn’t really do anything, I don’t think, to get ready for CPCI. It just seemed like CPCI was a direction that we wanted to go in.
Angie: well, we were already in that direction for the ACIC, we were managing chronic disease, where we were actually looking at chronic diseases, population health. What happened was we took the staff that we had at that moment, and said ‘OK, your job as you knew it, is gone. As a nurse, you are no longer going to room a patient, take vitals, and pass it onto the physician, you are now going to be actively involved in this care.’ And so we took the staff that we had at that moment and retrained them to meet the needs of how we wanted to manage at that time.
Brian: You mentioned care planning, and that’s the next topic on this list — planned care for coordination of chronic conditions and preventive care. How did you go about doing that?
Angie: So, we’re very big on team-based care. Everyone must practice at the top of their licensure. Dr. Walker has standing orders. So it starts at the front desk, when the front desk checks that patient in, she can see — this is a high-risk patient, and so it just moves onto the rest of the staff. The nurse knows when she pulls the patient back, ‘Oh, I’m sorry, this is a diabetic patient, I’m going to look over here in your CDSS alerts, I’m going to see if you’ve had your foot exam, your eye exam, your microalbumin. They’re actively involved in that planned care, and our planned care starts with — I think we identify with the top 10 diseases or diagnoses in the clinic, and then create standing orders for that. So it empowered our staff to start helping with that planned care, because one person can’t do that.
Brian: That’s great, that’s a wonderful way of approaching it. So, continuing on with that thought of planned care, do you use care plans?
Angie: We do. There is a wonderful initial care plan that comes with our module, that’s a very extensive care plan. We use that for our high-risk patients. We then went on to create our “shortie care plans” for our medium- and low-risk patients that are not necessarily disease not diagnosis-driven, it can just be a health part of it. You know, you come in and what they’re looking at — you need to increase your exercise, or decrease your weight and stuff like that. So we’ve created several to match our practice demographics.
Brian: Risk stratification. You mentioned you’re identifying risk up front. I guess the management part of that is really the question with risk stratification management. How do you go about handling that?
Angie: So, Dr. Walker created a risk stratification tool before we started CPCI. That tool was based on disease, where you’re at in your disease, and also your utilization in services. So when we came into eCW, we were able to create that tool into the note, so that when the nurses pull those patients back, they automatically risk stratify them every time.
Brian: Do you send them scores? Risk scores?
Angie: Yes. Ours is low, medium and high, but it’s based on a numerical count, as far as how they’re answering questions. Of course, once you pop into that high risk, there’s then other steps that we’re going to do within the practice to start helping look at those patients.
Brian: Patient engagement, patients and caregiver.
Angie: So, this was like my baby, I think. I love this one. This was the reason why we left our old EMR is because we could not reach out and touch those patients, without them being in the office. With the old one, the only time we ever saw them was when they came in. With eCW, we were able to really ramp up patient engagement via the Portal, via campaigns, they’re able to email the nurse, and they’re able to email the front desk. It was just my favorite, it was the whole point of what we’re doing. And we were a little worried at first because when we popped in, we were stage two, year two. So we were a mandatory 90 days. And so we did, I guess what you guys would call a “rip and replace” in August, so we had to hit everything come October, November, December. And so this was the moment we were worried about, and we blew it out of the water. Patients just loved it, they were very actively engaged in the office and what was going on, and being able to get onto that Portal, and be able to look at things and ask things — it was awesome.
Brian: It’s interesting when we’re talking about patient engagement, along with some of the other topics that we hit so far, a lot of them seem to run parallel to Meaningful Use. So, for example, with your patient engagement, being able to speak electronically with the patient, patients speak electronically with you that meets Meaningful Use measures, as well. Coordination of care across the medical neighborhood.
Randy: eCW has provider-to-provider referrals so that all of the results from EKGs and CTs and laboratory are sent directly from provider to provider, if you’re both users of eCW.
Brian: Which helps because you’re not going to have duplicate tests. So that’s a very big cost savings piece as well.
Angie: I would just say that we’re very actively involved in our community, so one of the big things that we did is we sat down with home health, we sat down with the hospital, and we sat down with different agencies, and said ‘OK, this is how we’re going to manage our patient. This is what we expect as far as care goes for our patient. And this is what we expect from you.’ And we continue those meetings — we have biweekly home health meetings, we meet with DME, we just want to make sure that everybody understands where we’re at, where we want to be and what we want for our patient. So I think, as far as coordination of care across the medical neighborhood, I think you have to really look at your neighborhood, and engage those businesses that are in healthcare as well.
Brian: Right, making sure that everyone is on the same page. That’s fantastic.
(Commercial Break)
Brian: Hi, welcome back, we’re here in De Queen, Arkansas with Dr. Randy Walker and Angie Walker, and we’re talking about CPCI. We just finished talking about the five functional areas that CMS was looking at, but there were also an additional nine milestones that were involved with that. I understand that those change from year to year, the different components, is that the case?
Angie: There wasn’t really that much change. I didn’t notice that much change. The milestones, to me, relatively stayed the same. Your reporting might have changed a little bit as you move through the years, but the milestones were always the same.
Brian: What sort of challenges did the milestones pose for you?
Randy: I think getting patients to participate in their own care, to take responsibility for their own disease, that’s probably the hardest part — which is the hardest part in all of this.
Brian: Across the board, that’s going to be the most difficult.
Angie: I would say for us, we were used to studying measures and looking at numbers and pulling out fallouts and trying to figure out where there’s issues and what we need to work on. So we already had something in place where we were monitoring, and so that just became a normal extension for us, as far as we’re going to meet this week for milestone two, or we’re going to pull the facts from shared decision making, or what have you.
Brian: You have that wonderful whiteboard in your office, that I find to be just genius, so that at a glance, you can tell where you stand with your different CQMs, which is an inspiration for folks that work in the office, to make sure they’re doing them correctly. And as you mentioned, it’s seen by patients, so that they know that this is a level of quality of care that they’re receiving. I think that’s a great, great idea.
Angie: It was important to us. At first, we were a little bit nervous, about putting ourselves out there. Because we did put it in a very public area, but we also realized that there are some measures that we simply can’t meet without the patient being involved. You know, we can set a goal of 30 percent of our patients receiving a mammogram or a colonoscopy, but if patients don’t participate in that we’re never going to reach that goal. It was important for us for the patients to see that they had a level of responsibility in meeting that goal as well.
Brian: Sure. Now, reporting on those measures. Did you self-report those, did you self-attest? And how difficult was that? I’ve seen some of the forms, and to me, honestly, it looked kind of convoluted. But tell me if I’m wrong.
Angie: I didn’t have a problem. I don’t feel like we had a problem with it. Of course, I have a CPC coordinator, that she and I chit-chat once a month on the phone. We pull measures every month that are put into my dashboard by the 10th. She and I have a standing conference call the Thursday after that. We look at what’s going on with those measures, where we need to be working on things, if there’s anything that needs to go on. And so when we get to that reporting period, we’re actually very familiar with what’s going on. With CPCI you report on a quarterly basis, so you know early on if you’re having issues, and you can correct those. And so when we get to that quarter, it’s good data, we know what we’re looking at, we know that it’s good, and so it’s just a matter of taking that information from the dashboard and putting it into the reporting module.
Brian: That’s a very good segue into my next question, which is, what sort of assistance did CMS offer you when you got involved with the program?
Angie: So, what they have is Transfer Med comes in and they do a lot of monthly webinars on just different topics that we’re looking at, whether it be medication management or shared decision-making. There’s all kinds of little different groups that meet, and there’s probably at least two or three webinars a week. We also have what is called CPC Connect, where we can actually go out and it’s almost like a Facebook platform where we’re able to talk with other clinics and figure out things that are going on and what have you. We also have our own Transfer Med rep, so that anytime we have issues they will come on-site to help us move through the obstacles that we might have, or if we have reporting questions or what have you, we can reach out to them.
Brian: That’s great. So they really did provide quite a deal of assistance since you’ve been doing this program. That’s fantastic. So, you mentioned earlier on that you were using another EMR when you began the program, and then moved to eCW. My original question was going to be ‘What changed in your flow, if you were using eCW from the full time of using the program.’ But really what I want to know now is, were there any particular functionalities within eClinicalWorks that you found to be particularly helpful in meeting the measures and meeting the core functions?
Randy: Well, from just a practical, day-to-day point of view, I love the way eCW has variable portions and constant portions. I’m really big on using the yellow stickies, the pink stickies, and then the variable portions of the care plans. It allows the nurses, the care managers, the other providers in the clinic to communicate with each other quickly.
Brian: And it’s right there when you look at the notes. You don’t have to search for it, it’s just there, right up in front of you.
Randy: Exactly.
Angie: And I think I really like the ability to track things. I love data. And so, being able to map things, and look at different things. You know, one month we did a study on PT and INR and we were trying to figure out if this piece of education helped better over another one, and so the ability of for you guys to create an area for me to map, and to be able to track numerators and denominators and know whether something we’re doing in the office is making a difference, is just awesome to me. You know, I can actually really know, versus, I’m going to ask the nurses and they’re going to say ‘Oh yeah, it’s good. Oh yeah, it’s good. Everything’s good.’ But when you actually can run that measure, or run that question, and you have data right in front of you, I mean, there’s no arguing with that. So, you know.
Brian: The old saying ‘You can’t manage what you can’t measure.’ And that’s absolutely the case.
Angie: And my think is, it allows us to measure what matters.
Brian: Overall, your experience with the program has been…?
Angie: Love it!
Randy: Yeah, we love it.
Brian: Well, thank you guys so much for talking with us today, we really appreciate your time, and the energy you put into the interview. It was really a wonderful experience talking to you, so thank you. Meet us again next time for more eCW Pocasts. You can find them on YouTube, iTunes, and my.eclinicalworks.com. Thank you for joining us today, and we look forward to seeing you again.