Published on Wednesday November 1, 2017
Healthcare produces lots of patient data, but practices and payers aren’t always on the same page. In this live eCW Podcast from the eClinicalWorks National Conference, Rohit Shinde from the healow Insights team joins host Brian Saal to discuss how medical record retrieval and closing gaps in care can help health plans reduce overhead costs, improve compliance, and boost Star ratings.
“It’s all about empowering the provider at the point of care. Build a product that adds value to providers and payers, but at the same time, the intangible outcome is patient satisfaction.”
Rohit Shinde, Business Unit Lead, healow Insights

Topics From This Episode
Discrete EHR Data
Everyone knows healthcare is shifting from a fee-for-service to a value-based, or “pay for performance” model. But what impact does that have on payers? It means they are looking beyond basic claims data, in search of discrete, actionable EHR data that can help them improve compliance and improve outcomes for their members. It turns out that not all of a patient’s key information is covered by ICD-10 and CPT codes.
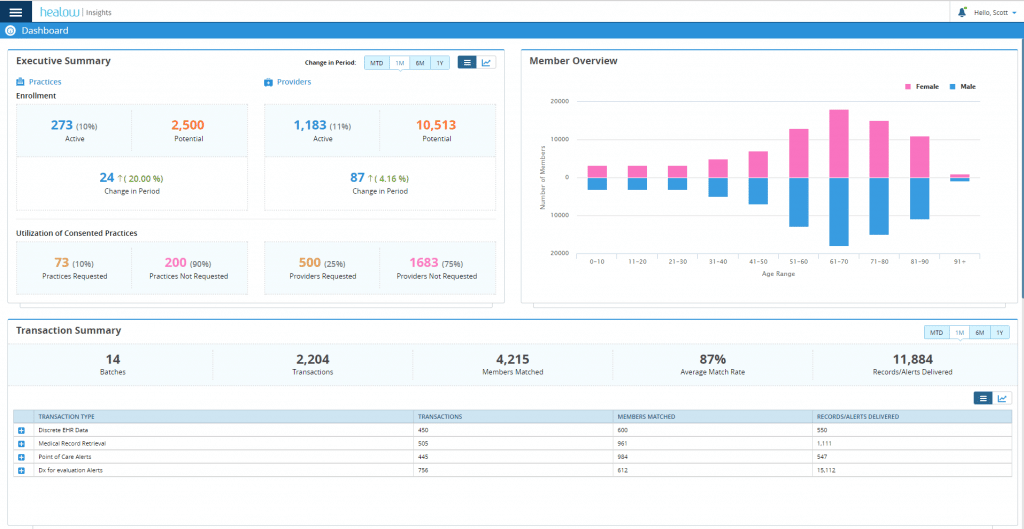
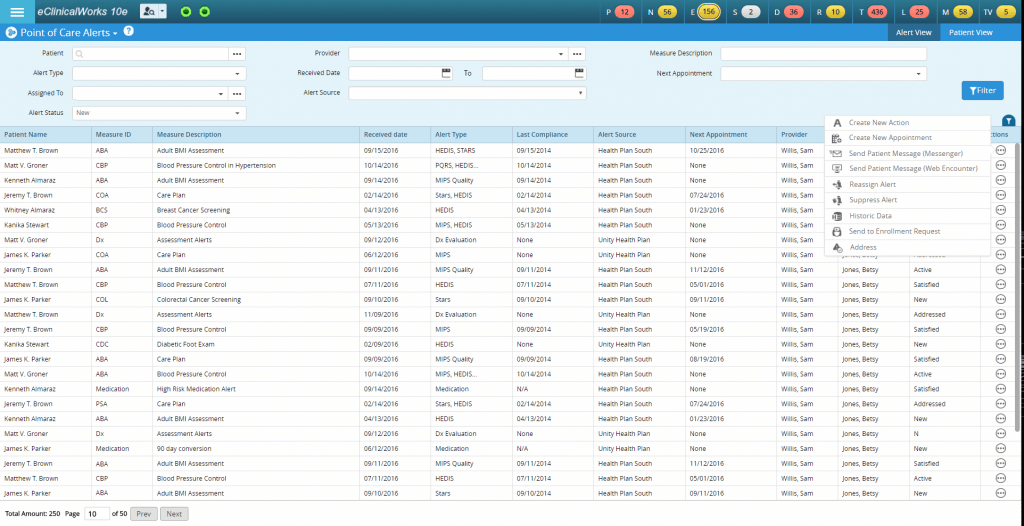
Point-of-Care Alerts
Today’s practices have lots of patient information, and lots of ways to engage patients in need of regular screenings and checkups, including alerts and reminders. Meanwhile, today’s patients today move around a lot, seeing their primary care physician, along with specialists, and perhaps having screenings elsewhere. Helping track, resolve and manage those alerts is a key part of the healow Insights solution.
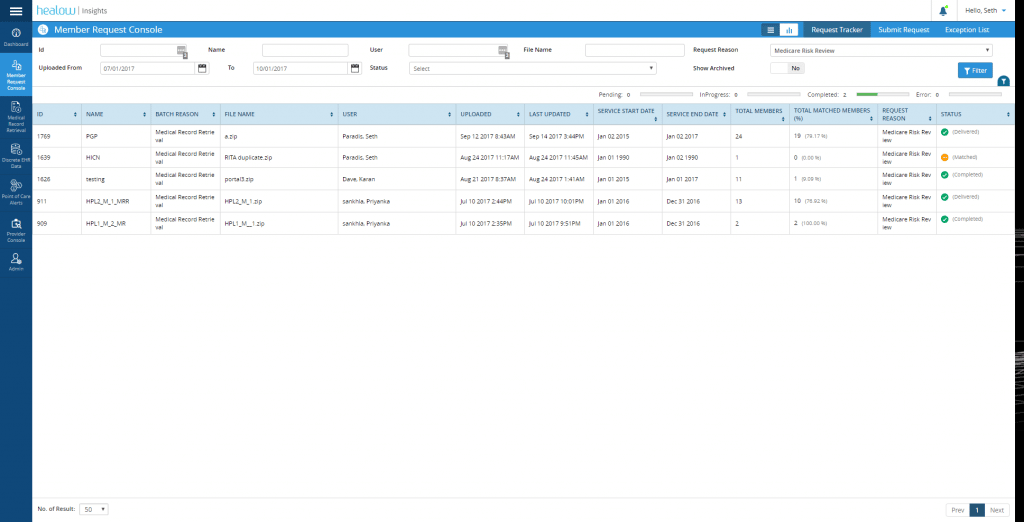
Medical Record Retrieval
Electronic Health Records for documentation are great tools, but practices, patients and providers come to healthcare with differing perspectives. And when multiple EHRs and reporting methods come into play, the result can be gaps in knowledge, information, and care. With fast, effective methods for Medical Record Retrieval, healow Insights helps keep the focus on adding value for all providers and payers, while at the same time ensuring that patients are satisfied.
Transcript:
Brian Saal: Good afternoon, and welcome to another edition of eCW Podcast. We are coming to you live today from the 2017 National Users Conference here in Dallas, Texas. With me today is Rohit Shinde. Rohit is the business leader of a new area of eCW called healow Insights, and thanks very much for being with us today, Rohit, we appreciate it.
Rohit: It’s always a pleasure, and joining you on the 10th-anniversary edition of our Users Conference is always a proud moment. So, thanks for having me.
Brian: It’s a very exciting moment, the 10th anniversary. So, bridging the gaps between payer and provider is the underlying title of healow Insights. Just discuss a little bit what the challenges [are] that a practice might face in bridging that gap.
Rohit: And that’s, again, the whole premise of this business unit, is how can we add value to the provider side, and empower them to provide optimal care delivery to their members, by empowering them with the information from the payer, and vice versa, where we dig deep and we see today that there are so many challenges, so much heavy lifting, so many less efficient workflows that happen today, when we talk about fraud, waste, and abuse in the healthcare delivery system. So, think about it simply as: We started out as eClinicalWorks, which providers are using in their practices as their EHR.
Brian: Sure.
Rohit: As we say, that’s our core. We added the Patient Engagement aspect on top, which is through healow health and online wellness, which, again, helps practices connect with their patients, right, consumers. And the extension of that is now healow Insights, which is helping the practice connect with the third “P,” which is the payer.
So, think about the ecosystem of eClinicalWorks and healow, helping connect the providers, the patients, and the payers. And that’s again, when you look at the challenges between payers and providers, there’s a lot more happening. And the fundamental reason we see these challenges happening now, versus 10 years ago, is because the evolution in the reimbursement models. Things are shifting. The earth is moving from fee-for-service to pay-for-performance.
Brian: Right.
Rohit: And that’s where payers are looking beyond claims data. They’re looking for actionable information, they’re looking at discrete EHR data that can help them be more compliant, and improve their quality outcomes for their members.
Brian: So, it sounds like that the information that can be provided back to payers is not claim-based, necessarily. We’re talking about structured data. Is that accurate?
Rohit: Exactly. And that’s, again, the whole ballgame on the quality aspect side of healthcare, revolves around improving outcomes, reducing costs, and making sure the customer is satisfied. So when you look at the customer, and that’s really the premise of healow Insights, is consumerization of healthcare. That’s what the payers are focused on, that, as a consumer, are the providers satisfied? And as a consumer, is the patient satisfied? So much of the heavy lifting when it comes to accurately doing chart audits, accurately identifying certain care gaps where care was delivered — because they didn’t see that in claims, it was not an ICD, it was not a CPT — how can the payer get that information on demand? And how can the practice then be rated, or scored, to their fullest potential, versus getting quality scores just based on the ICDs and the CPTs that are submitted in the claim. And that’s where they see that they fall short, even though they are providing care at 80th or 90th percentile, they get three-star rated, and again, reaching for the stars is the whole game over here.
Brian: So, when we’re talking about stars, of course, we have to bring up HEDIS. And this is an added benefit to help providers to make sure that they hit those HEDIS scores as they go along.
Rohit: Absolutely. Complements, exactly, with our provider tools, which is the HEDIS dashboard on the Population Health side. So, they use that as a GPS to navigate their compliance, based on the data sitting within their EMR. Now, what we are trying to do is bridge the last mile, is to make sure that the scores that they see on behalf of the participating practices, we can report that directly to the payers, so the payers can also attest to the same level of performance that they are meeting, versus what is truly non-compliant, what is truly outstanding, and then they can start pushing those actionable care gaps back into the practice, into an integrated workflow, so care is proactive and not reactive, which is what we see today.
Brian: So those are being addressed immediately, rather than waiting a month or however long down the road, to be actually moving on them.
Rohit: You’ll be surprised. So, there is a conception called “HEDIS season” in the practices and payers today. Again, inefficiency-wise, it’s so big, they don’t want to disrupt the practice — obviously it’s adding cost and time to both parties involved, so it’s done once a year. And that’s the whole game-changer, that through healow Insights we are making it on-demand for both the practices and the payers and it can be ongoing, rather than just being once a year. And that, I think, is a great way for providers and practices to take advantage of healow Insights. The reason being is, one, it is at no cost to the practice — it is part of your eClinicalWorks product line, and part of the core — and second, things that they could imagine doing once a year, because of the efficiency and the productivity loss, they can now do it on demand, without having the need to leave their office space, or having third-party vendors coming in and doing these chart audits.
Brian: That’s interesting, because I was going to ask you about chart audits, and how this sort of changes the game in how chart audits are performed.
Rohit: It makes it, in fact, more compliant, and very, very much streamlined. The reason it makes it more compliant is today, think about third-party vendors who come to your practice. They may come every month. They may come every quarter. They come and say, here are 400 patients that we need to audit, and practices pretty much don’t have the manpower or the bandwidth to hand-hold them, so most of the time they will just give them a login to the EMR, and say spend four hours, and take what you need. And that, I think again, from a HIPAA compliance standpoint, you are basically opening the whole EMR to them.
Brian: Very true.
Rohit: So, many practices want complete visibility and transparency to the whole process, so in fact we have a proprietary matching algorithm, and this is a request-based model, so once practices opt in, payers request — let’s say they want to audit 20% or 40% of the claims — they send a request file, or a chase file, is what they refer [to] it as. Using that file, we are able to accurately match members. It’s a matching algorithm. If it fails, those are listed as exceptions, just as today lab results come in and don’t match, those go into an exceptions bucket. But if matched, then we are electronically able to look at the locked flag of the Progress Note and send the chart seamlessly and directly into the payer’s SFTP folder. So, again, it makes it seamless. There is no hand-holding. On average, we are seeing practices getting 0.5 to 1.0 FTE back to do their own stuff, and talking to enterprise customers, they are saying, ‘Hey, we were investing $50,000 to $60,000 in our IT budgets to just handle such requests, because the volume goes up when you have many practices, and even IT resources. So, CIOs basically are saying this is awesome, because I can get that same budget allocated to focus on other things, and I can have my resources back to focus on other projects. So, it’s a win-win scenario for both the payer, where it’s being more efficient and timely and accurate, but for the practice, as you said, it makes it productive.
Brian: Certainly, the time commitment that a practice, and particularly a large enterprise practice, has to put into this can be really, really extensive. And so, that slows down productivity back at the practice, but it also slows down the payer’s productivity, because they have to wait for this information to be generated and brought in, so this is really just kind of a push the button and off it goes.
Rohit: I would summarize it saying things that practices or payers could imagine doing once a year, or twice a year, or every quarter, they can do it proactively every week. A patient walks in, is seen by the doctor, payer gets the data of what was seen. Payer can push care gaps the following week, saying ‘Hey, Brian was there, you gave him a flu shot, but you forgot to follow up on his colorectal cancer screening. And he was overdue for it.’ Rather than sending that information, saying ‘Hey, practice, you have 500 patients that are overdue for a cancer screening,’ at the end of the year, which is putting the practice behind the eight ball —
Brian: And on the patient as well. I mean, that’s definitely detrimental to patient care, particularly, as you mentioned, with something, like colorectal cancer screening. You want to catch those as quickly as possible, and putting them off even six months could be potentially detrimental.
Rohit: And it actually will work wonders when it comes to more outcome-based measures than your traditional preventive screenings that I just gave an example of, and again, especially with care of adult adults, medication adherence — these are real-world scenarios where the outcome is not an order, the outcome is not a lab value, the outcome is not a medication. It is goals that you are defining and following through with them. And those goals are what even payers and providers want, is to move away from illness-driven episode, which is an encounter, to more of a wellness-driven outlook. And that’s where the game changes with healow Insights, is the payers want to empower the practice, the provider, with the 360-degree view of the patient’s data. Payer has everything — inpatient, outpatient, pharma, DME — anywhere you pay with your insurance card, that information is important, and that data coming back into the four walls of the practice, into the eCW database, makes a huge value-add for the practice when they are talking about care delivery for that member.
Brian: That’s exactly one of the next questions I wanted to get to in terms of benefiting the practice. How does the practice view that data? How does it access it, so to speak?
Rohit: So, seamless and actionable. Those are the two benefits, I would say, speak right off the back. And then the third, which I already mentioned, that from a cost perspective, this is not an added line item for the practices to pay, it’s integrated into their EHR workflows, it’s part of their EMR license fees. The only thing is, it depends on the payers to be ready to start pushing that data back. So, seamless, because today it’s disruptive. Payers have this information, they share it with practices, but it’s a very disjointed and disconnected workflow. They tell them ‘Go to this website, you will see all the patients that are open for care gaps, or overdue for certain measures.’ They may send it on a spreadsheet. They may send it to different things. They may send once a year, they may send once a quarter. So, again, it’s all over the place. And when you talk to a practice, which is one of the challenges we spoke about, was, a practice on average has four to five payers that they would meet with on a day-to-day basis, so think about 25 different methods we have to keep in mind, in addition to seeing 20, 30 patients a day and documenting that data in the EMR. So, it’s again, a very disjointed process, because of which practices are not taking advantage. That compliance in the long run hits their quality scores, which again, today is tied to pay-for-performance.
Brian: Absolutely, so very important today.
Rohit: So, it’s integrating it, so they can consume it seamlessly, part of their day-to-day workflows in the EMR.
Brian: Directly from eClinicalWorks?
Rohit: Exactly. So, think about your CDSS Alerts. Today, CDSS Alerts shows you any alert that is generated based on the data sitting in your EMR, in your practice, that you capture. Think about the same CDSS tab now expanding to also include payer-generated alerts, or gaps in care, so when you’re technically a member, your patient, you’re able to hit it at the same time, saying, according to this, it shows me you’re overdue for X, Y, Z, but your payer also wants me to focus on care of older adults, which is screenings and other things I need to do.
Brian: Does it provide other data on the patient in the sense that — you know, we were talking about CDSS Alerts. Let’s say that the patient’s a snowbird, and is down in Florida during the winter, and you’re seeing him in the summertime. And in Florida he’s had a colonoscopy. Is that information going to be transmitted back?
Rohit: Absolutely, and that’s the big picture. Interoperability is a key over here. As a payer they know the 360-degree view. You went to Florida and had a colonoscopy over there. You went skiing to Colorado and you broke your ankle over there. Your primary care sitting in Boston may not know all these things, or may not think about connecting and getting that data from Carequality or CommonWell. So, as a payer, they want the PCP who’s in Boston to own the care of this patient. And that’s the data that, as a payer, they can share which is member summary, or member insights, which will also be brought into the left-chart panel of eClinicalWorks, and you can see data around ambulatory care, acute care, pharm, DME — everything that the payer is focusing on.
Brian: So, now we have the really great power of being able to gather data using CommonWell and Carequality, and certainly with the new on-demand capabilities within eCW that makes it even easier. But I think this is interesting because you don’t even have to know that this patient went to this particular practice to get this data, and that data can come in to you, and then if need be you can go out and connect with Carequality. But that data is going to come in nonetheless. You’re going to get a full and complete picture of the patient at the time.
Rohit: Exactly. And that’s where your EMR may say ‘Hey, Brian is overdue for a colorectal cancer screening,’ but if that patient had gone to Florida, had gotten it there during the snowbird season, that information can come back, to then say, ‘Hey, the patient is already compliant for this.’ And you will be able to import this. The whole goal at the end is to integrate this data into the pre-visit planning that Dr. Raj spoke about this morning. It’s about integrating it into the practice workflows, not just for the provider when they are in the room with the patient, but also through our T Jellybean actions/workflows, so there are clinical staff or nurses, who can be more proactive, and for some of these measures they can call the patient, find out what are the goals, what are the case management things. And many of our practices are taking advantage of those episodes also.
Brian: And pharmacy, as well. So, again, if you have an easier way of filling out or understanding the full, current meds of a patient, does it also give you a little bit of that history as well?
Rohit: Yeah, so that’s a very good point. Because, with pharmacy, we’re actually going to start expanding next year into two phases. One is, we want to help providers understand the proportion of days covered — which is called medication adherence. So, I go to the doctor once a year, I may go to the doctor every quarter, depending on my conditions. The doctor leaves me with medications, there are four refills in it, 90 days’ supply. The doctor doesn’t know if I go and pick it up. The payer knows, because the pharmacy sends them a claim. So, depending on when they are picking up — so if it took you 100 days to pick up your first refill, then what did you do for those 10 days when you didn’t have any medicines or, you didn’t take it. So, proportion of days covered is, again, a measuring yardstick that payers look at from an adherence perspective. CMS is very gung-ho on medication adherence also, which is we want to make sure a patient has drugs when he or she needs it. That Insights is going to help the provider to say that ‘Hey, I’m going to see you after six months, and I can really see how you are being adherent to your medication treatment. Have you been picking up your medications on time? Have you been taking them?’ And the second aspect which we see from a pharmacy perspective, and this is again talking more consumerization of healthcare, is, how can we help patients know what their out-of-pocket costs will be? That’s, again, a new concept which today, at the point of care, when the provider is prescribing Lipitor through CVS pharmacy on Main Street, I as a patient have no clue what my out-of-pocket cost — I’m not talking about average wholesale price, I’m talking about out-of-pocket cost — will be when I go pick up the medicine at CVS. It’s more like a ‘Drum roll, please!’ and then the pharmacist will say ‘Rohit, you owe $45 or $120 for this medication, and my doc never told me that, is what I’m thinking! So we want to reduce that burden and make it more consumer driven, where we would like to get that API built with payers, so that while you are in the room, we can bring more insights from the payer, empower the doctor to say that ‘Hey, if you go to Publix, the same drug is covered at no cost, because it’s in your insurance coverage, but if you go to a Tier 1 pharmacy, it’s going to be $15, and as a consumer I can say ‘Thank you, doctor, for saving me that copay.’
Brian: It’s interesting when we talk about pharmacy and meds, because we are so interested in med reconciliation within our own record, but it’s also so important to make sure that the patient is compliant with what we’re asking them to do. And if we don’t know that, if we don’t know that they’re not compliant, we can’t adequately treat what the condition is.
Rohit: It’s all about empowering the provider at the point of care. And I think that was the whole venture when we started onto this journey. Our CEO basically said: ‘Build a product that adds value to providers and payers, but at the same time, intangible outcome is patient satisfaction.’ So, coming back to the three P’s that we started off, saying ‘Hey, we have the provider, the patient, and now the payer,’ that’s exactly our journey, to connect the dots and bridge the gap between payer and provider by identifying what are the challenges where we can exchange data both ways.
Brian: Both ways, and this really is ground-breaking. I don’t know of anything else out there that, again, does bring you full-circle with that data. As you said it a little bit earlier, it’s a win-win for everybody. Everybody gets something out of this, and the cost is, I think you mentioned this already…
Rohit: It’s a whopping zero cents for the provider and the practice. And again, the goal is simple: We want to make sure they are more compliant. We know that compliance results in higher scores, higher reimbursements, because CMS — and this is a fact — that half a Star rating the payer goes up, CMS pays $40 more PM/PM to the payer. At the end, based on the contract, providers have in their plans, 80% of that money goes back to the provider. So we do not advertise this that practices or payers will be making more money or anything, because we know if we empower them to get the job done, make sure the insights are there, it’s more proactive care rather than reactive care, it situates them in the position to succeed in taking care of the patient, in keeping them healthy, reducing the fraud, waste, and abuse of the healthcare system, and that, I think, will easily result in higher scores, higher ratings, which in turn will be linked with higher reimbursements in the long run.
Brian: And improved patient care.
Rohit: Absolutely.
Brian: Improving healthcare together.
Rohit: That’s the intangible outcome. The patient as a consumer is going to thank the health system. Because today, when you talk to patients, we all are consumers in some shape and form when we fall sick. And when you talk to them about healthcare, those two words, health and care, scare some of us sometimes. And I think what funnels us, what fuels us to take on this innovative journey with healow Insights, where we are trying to connect between the practice and the payer, to identify what are the use cases, what are the challenges that can innovate, and make consumerization of healthcare possible.
Brian: Thank you so much for giving us that insight into Insight — I had to make that pun! Is there anything else you’d like to add?
Rohit: No, I think, this is again a new journey, so I urge practices to dig deep, talk to their payers who are looking to innovate, and take the next step into data exchange through healow Insights. Bring those leads to us, talk to us, so that we can engage the practices on behalf of these payers, so that we can facilitate building these bridges between the payer and the provider.
Brian: Is there an email address folks could use to reach you?
Rohit: Yes, they can use payeralliance@healow.com
Brian: Great. Thank you, so much. Everybody, thank you for joining us for another edition of the eCW Podcast. Again, we are here live from the Gaylord Texan in Dallas. Keep in mind that you can always find more eCW Podcasts on YouTube, iTunes, and my.eclinicalworks.com. Again, thanks for joining us, and we’ll see you again very, very soon.

