MIPS
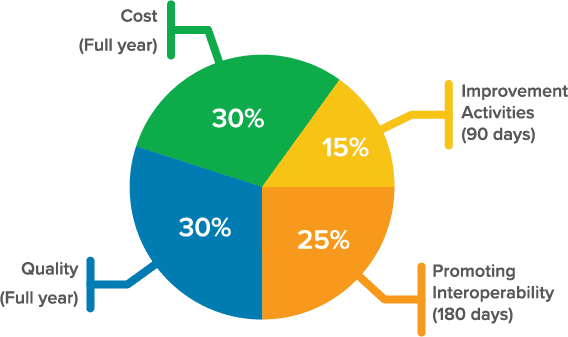
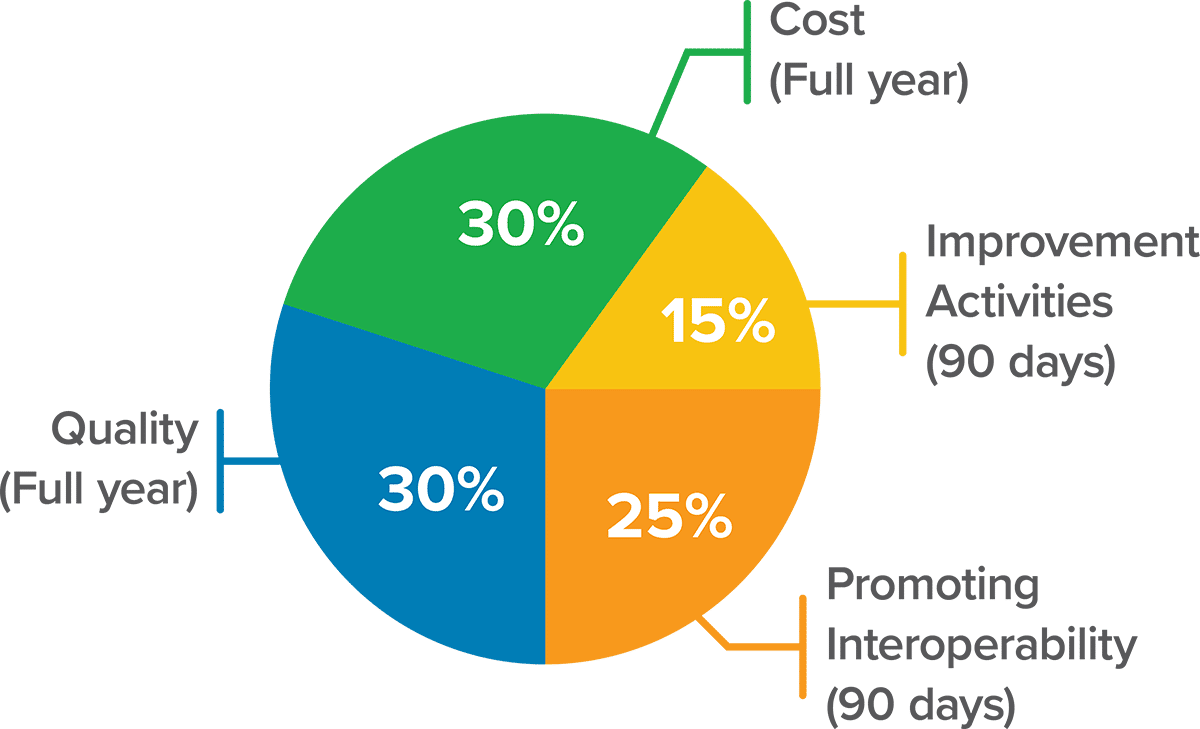
Most providers will be subject to MIPS — the Merit-Based Incentive Payment System, which consists of revised performance categories:
On January 1, 2017, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) reformed the Medicare physician payment system through the creation of the Quality Payment Program, rewarding Medicare providers for the quality and value of care patients receive, rather than for the volume of services provided.
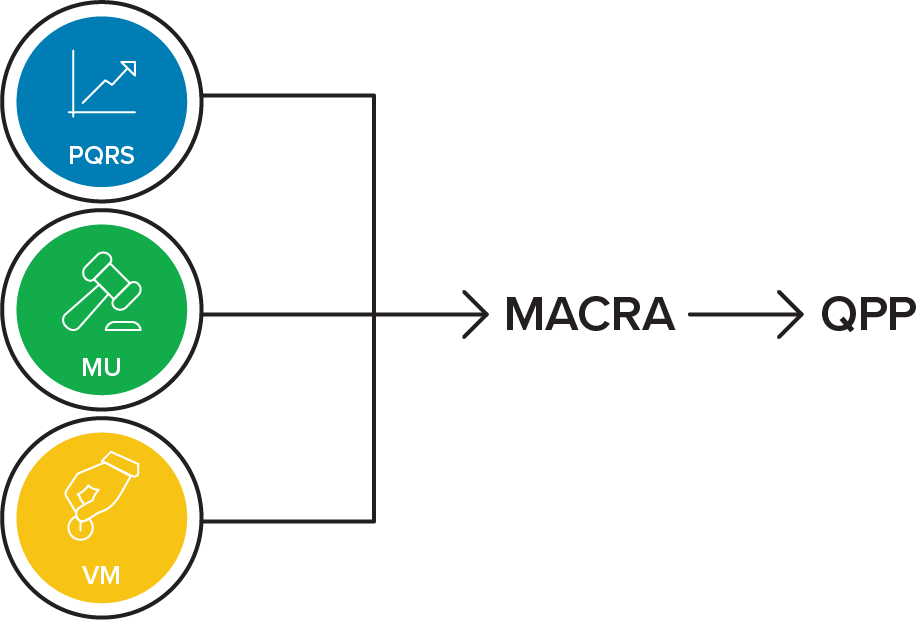
Most providers will be subject to MIPS — the Merit-Based Incentive Payment System, which consists of revised performance categories:
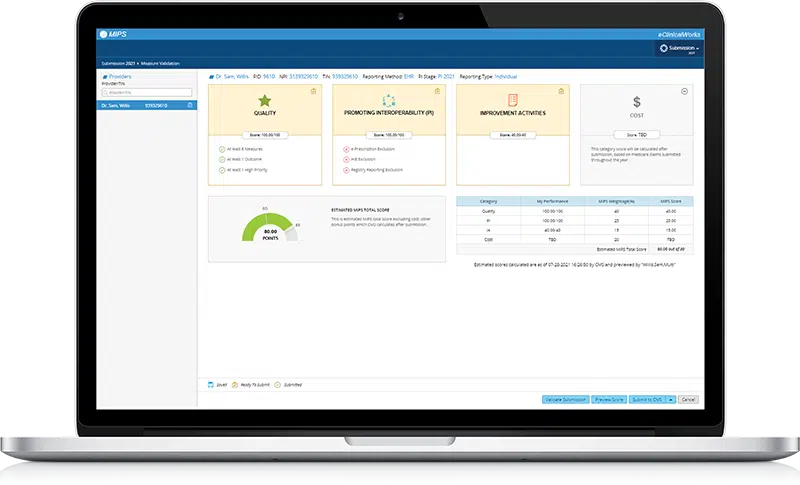
eClinicalWorks can help you navigate every aspect of the new requirements. Our experts have the experience and knowledge you need to choose the right mix of quality measures for your practice.
2025 Performance Year

MVPs are the newest MIPS reporting option (an alternative to “traditional MIPS” and “APM Performance Pathway (APP)”) that you can use to meet your MIPS reporting requirements.
There are several participation options for the MVP method. Providers can report individually, as a single specialty group, a multi-specialty group, a subgroup, or as part of the APM entity. A subgroup would be a subset of providers that are a part of a larger group under the same Tax ID that could form a smaller subgroup to report data for that set of providers.
Providers or groups must register between April 1st – November 30th of 2024 indicating which MVP they plan to report and the providers who are part of the group. Under MVP reporting you would still be responsible to report the same four performance categories as MIPS, but with slightly different requirements.
APMs, or Alternative Payment Models, offer additional incentives to practices that adopt risk, provide high-quality, cost-efficient care, and meet certain conditions.


Advanced APMs are for practices who are willing to take additional risk based on their patient outcomes. Qualifying Participants (QP) participating in Advanced Alternative Payment Models (AAPM) can earn a 1.8 percent incentive for performance year 2025, and a higher Physician Fee Schedule update for performance years 2025 and beyond.
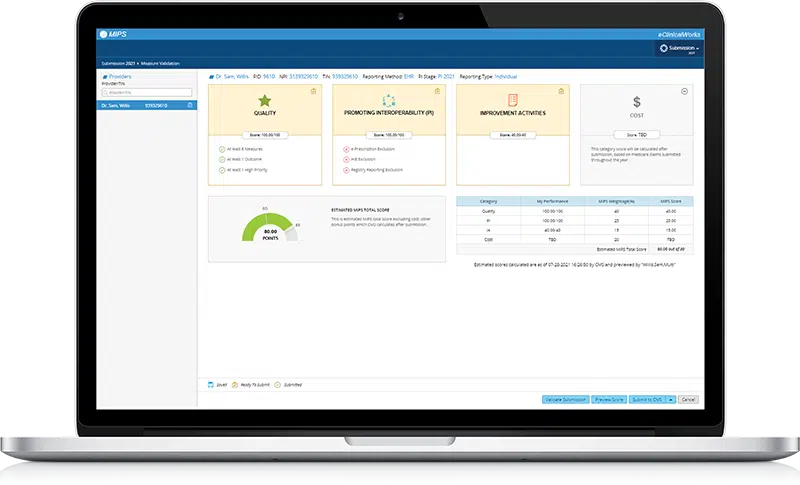
eClinicalWorks helps customers meet complex MACRA/MIPS requirements with free videos, webinars, and documentation. Our consultants work with individual and group practices to navigate the complex regulatory environment in the transition to value-based care, including:
“I had the pleasure of working with my eClinicalWorks MIPS consultant. Without her expertise, I could not have achieved the remarkable scores and incentives I did. She was readily available to answer any questions. I would not want to even attempt to deal with MIPS without help from my trusted eClinicalWorks resource!”
Terry Goldblatt, Center For Dermatology
Most providers will be subject to MIPS — the Merit-Based Incentive Payment System, which consists of revised performance categories:
eClinicalWorks can help you navigate every aspect of the new requirements. Our experts have the experience and knowledge you need to choose the right mix of quality measures for your practice.

MVPs are the newest MIPS reporting option (an alternative to “traditional MIPS” and “APM Performance Pathway (APP)”) that you can use to meet your MIPS reporting requirements.
There are several participation options for the MVP method, Providers can report individually, as a single specialty group, a multi-specialty group, a subgroup, or as part of the APM entity. A subgroup would be a subset of providers that are a part of a larger group under the same Tax ID that could form a smaller subgroup to report data for that set of providers.
Providers or groups must register between April 1st – November 30th of 2023 indicating which MVP they plan to report, and the providers who are part of the group. Under MVP reporting you would still be responsible to report the same four performance categories as MIPS, but with slightly different requirements.
Finalized MVPs:
APMs, or Alternative Payment Models, offer additional incentives to practices that adopt risk, provide high-quality, cost-efficient care, and meet certain conditions.


Advanced APMs are for practices who are willing to take additional risk based on their patient outcomes. Qualifying Participants (QP) participating in Advanced Alternative Payment Models (AAPM) can earn annual positive adjustments of 5%.
eClinicalWorks helps customers meet complex MACRA/MIPS requirements with free videos, webinars, and documentation. Our consultants work with individual and group practices to navigate the complex regulatory environment in the transition to value-based care, including:
“I had the pleasure of working with my eClinicalWorks MIPS consultant. Without her expertise, I could not have achieved the remarkable scores and incentives I did. She was readily available to answer any questions. I would not want to even attempt to deal with MIPS without help from my trusted eClinicalWorks resource!”
Terry Goldblatt, Center For Dermatology