
Published on Monday February 4, 2019
Adult Medicine of Lake County, serving a largely geriatric population in a rural area north of Orlando, Florida, has successfully implemented interoperability solutions through eClinicalWorks. Exchanging patient data and tracking each patient’s history have been key factors in providing high-quality care to their patients, who include many seasonal residents; controlling costs by improving visibility and thus reducing redundant and unnecessary tests; and even deterring patients who may be seeking an office visit solely to obtain an opioid prescription.
“In the future, as we move to the value-based care and HCC coding, this gives us such a better-rounded view. We can see exactly what the specialist coded, and make sure we’re coding to the highest specificity. There are going to be a lot of intangible benefits.”
Matt Cady, practice manager, Adult Medicine of Lake County

Topics From This Episode
Interoperability
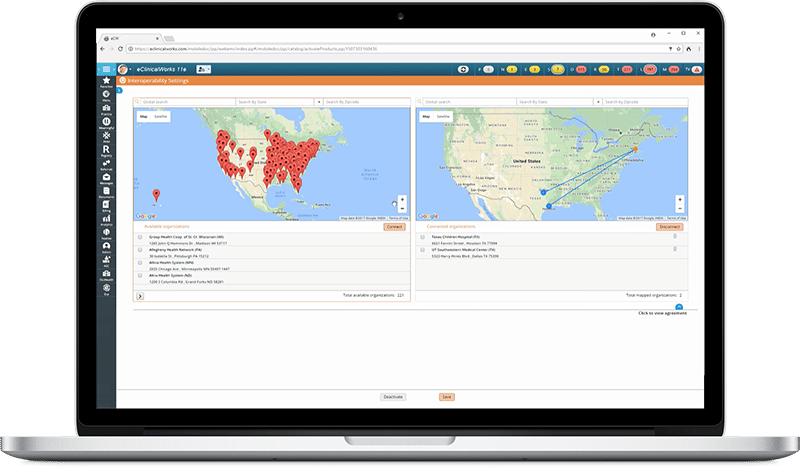
eClinicalWorks is committed to providing customers with affordable, state-of-the-art interoperability solutions to ensure that providers have complete visibility into each patient’s medical history, and all the data they need, on demand and at the point of care, to help promote quality care.
Brian Saal: Hello, and welcome to another edition of the eCW Podcast. Today we’re coming at you live from the 2018 eClinicalWorks National Conference here in the Music City, Nashville, Tennessee. I’m your host, Brian Saal, and with me here today is Matt Cady from —
Matt Cady: Adult Medicine of Lake County.
Saal: In Florida.
Cady: In Florida, outside of Orlando.
Saal: And today we’re going to be talking about interoperability. Thanks for being with us, we really appreciate it. Before we get started, could you tell us a little bit about your practice?
Cady: We’re right outside of Orlando. We currently have seven providers. Most of them are going to be Medicare. We’re right outside of the country’s largest retirement community, so we have a very interesting mix of patients.
Saal: And you are currently using CommonWell and Carequality to bring data into the EMR. Tell me, well, first of all, tell me how you went about setting that up. Were there issues that were involved in the setup?
Cady: I’ll go even a step back. It’s one of my favorite things, is once a week I look at the product activation screen to see what new has come out. So when we first saw this, it had actually appeared there before there was any literature, but I clicked on it. We wanted it. It’s a very easy, self-guided activation. We picked out the hospitals, the area that we were concerned with, and literally two clicks and you’re in. It’s actually become easier now, you don’t even have to pick the areas. As soon as you enter into it, it pulls every in.
Saal: We do know that there is the necessity of getting patient buy-in or patient consent.
Cady: Correct.
Saal: To use that. Do you use the opt-in or the opt-out method?
Cady: We use the opt-in, and we actually introduce this as soon as they register as a new patient. And one of the biggest benefits we found is, once they opt in as registering, when they first come in, we actually are able to pre-fill out all their record request forms, because we know everybody they’re already seeing, which cuts back a tremendous amount of time on the first visit.
Saal: Oh, well, that makes perfect sense.
Cady: I was going to say, it actually even helps fill in some gaps, because a lot of times patients won’t remember where they were six months ago, or who they saw a year ago, and using this we’re able to see literally a complete picture going back sometimes as far as 10 years.
Saal: Now it’s interesting you said that you’re working outside one of the largest retirement communities in the States. But do you also have experience with snowbirds, folks who are coming down from the north in the wintertime to —
Cady: Massive challenge. In fact, we have a huge influx, everywhere from the restaurants to our lobby, you’ll feel the influx of them as soon as the first cold front comes through. And that actually helps us, because to try and reach out to a provider we don’t know in Boston or New York — this is easy access. We have contact phone numbers, everything.
Saal: And, you know, the nice thing about it is it works both ways. So, if someone has an incident that takes place down in Florida, they come back up to Boston, and you know, Mass General or whomever can actually see that data your folks picked up on and be able to keep that continuity of care going the entire time.
Cady: Correct. And there’s actually another benefit that we realized. A lot of times we’re able to see the Problem List and what the other offices have coded for, so it actually educates us on what our specialists or even people we didn’t know they were seeing are seeing with our patient, and it gives us a more complete Note.
Saal: Oh yeah, sure, absolutely. You also mentioned a little bit earlier that you’re in a rural area?
Cady: A very rural area.
Saal: So, you really do need to be able to get information from hospitals that are from very diverse areas around the state, I would assume.
Cady: Correct. Because, like you said, with the snowbirds, we could from them from Montana to Maine and all the way over to Mt. Dora, so we never know where we’re going to be pulling the information from.
Saal: And yet that data is so invaluable to providers, to be really able to up the level of care that they’re giving to the patients. Do you do the pull of the data when the patient checks in or do you do it in the room? Where is it being done?
Cady: We do it during the pre-visit planning, so we’ll do it ahead of time.
Saal: OK.
Cady: And then we’ll pull it all in. We can collaborate. A lot of times, like I said, when you establish as a new patient, we’ll have everything ready even before you’ve had your first visit, so we’ll have a complete picture of that patient.
Saal: That’s fantastic. And that’s what it’s really all about ultimately.
Cady: Another — I didn’t mean to interrupt you — but another benefit we never even realized, obviously there’s an opioid crisis going on right now, and trying to identify the patients that aren’t really seeking care, but are seeking just an opioid, we’re able to look at this and see that they’ve tried to establish three or four times in recent time, and so what we realize is you may not it on E-FORCSE or the federal drug database, but we can see them trying to establish in numerous places, and it makes us question, hey why are we their same practice, that you’ve seen four new established visits —
Saal: Right, within the last two weeks. Yeah, well, identifying it, particularly in this age of the opioid crisis, being able to identify quickly and easily drug seekers is a lifesaving measure.
Cady: It really is.
Saal: So that’s a use that, frankly, I’d never considered, but it really makes absolutely perfect sense.
Cady: Another use we found is, with our marketing team, they’ll actually ask the patients different questions about why they picked our practice. So we’re able to judge the effectiveness. We do a lot with people moving into the area, we welcome to the area. And so, if we see that you’re recently relocated, we ask you a different set of questions. Because we know you didn’t read the [inaudible] paper, we know you didn’t hear it word-of-mouth, you’re new to the area. So, we’re actually able to judge our marketing efforts too.
Saal: Absolutely. Now, you also mentioned — well, I’ve mentioned this previously — that you have a lot of older patients coming in. And obviously, with some of our more, well, our older patients, they may have some issues in terms of cognition and in terms of being able to accurately describe things that have happened to them or medicines that they’re taking. I’m assuming that this is going to be a huge help for that, as well.
Cady: Huge help. Huge, huge help. We were able to identify, you know, they may not remember where they were six months ago. We can actually bring up the doctor’s name and say, ‘Oh, he’s over by Publix.’ And she says ‘Oh yes, I do remember going to him, now.’ So, it’s been a massive benefit there. And then also, like I said, when it brings in the Problem List from the other provider, it’s education to us. Because we respond to something we may not have responded —
Saal: And there’s got to be some revenue enhancement abilities with that. Not enhancements per se, but possibly some savings, in terms of being able to say, well, when was your last A1c. Well, I haven’t had one for six months. You go online, you look, you say, well, actually you had one last week, so there’s no reason for us to do it again.
Cady: Absolutely. There’s actually both cost savings and a chance for additional revenue. We’re doing a lot of cost savings now, because we’re finding as a primary, you may be going to see either another primary, when you should only be seeing us, or you may be seeing a specialist for a service that we could perform in-house, in which case we’ll educate you, and then you can just keep it in-house for a reduced cost.
Saal: Yeah, and that saves money for everybody. So that’s a great use. Now, you mentioned that you had a couple of use cases that you wanted to talk about?
Cady: Yeah, we’ve got a couple. So, we had a lady that literally just moved into our area, had a life-changing event and was put into the hospital. So, we had to do a, literally, a welcome to Medicare, welcome to the practice, in transition to care practice, but she hadn’t had a caregiver, and she really didn’t have a lot of history. So, being able to pull that data gave us a very accurate picture of what she was up against and where she had been. And so, even though she wasn’t able to articulate it, we were able to fill in the blanks for her.
Saal: That’s fantastic, because you know you do have a patient that comes in like that, that is a complete blank slate, and that really can’t help you that much in filling in the blanks there, but this interoperability will actually go out and fill in the blanks, so to speak.
Cady: Yes, and like you mentioned, it’s both ways. A snowbird that had returned back up to New England had an incident, and the provider up there said ‘We’re able to see,’ I mean the provider up there was blown away, he said ‘We’re able to see what happened to you in Florida.’ And she had actually called us and thanked us, and I said “Ma’am, we didn’t — it just does it.’ I said that’s just the benefit of what we do. So, it was really, really neat and you could see that it meant a lot to her.
Saal: Absolutely, absolutely. Was there another one?
Cady: The other one is probably not as encouraging. It was again, with the opioid crisis, we’re finding that people are getting better and better at kind of duping our front desk into allowing a visit to happen, and we were able to stop someone that was coming in for nefarious reasons. It was an eyeopener because all other methods we had didn’t trigger this. It wasn’t on the federal database, there wasn’t a lot of other things, but when we were able to pull his description, we could see that there were numerous office visits, and it didn’t make sense.
Saal: There it was. That’s great, that’s great. So, you know where we are with interoperability right now, we know the tremendous benefit that it’s giving to providers and patients across the board. Where do you see it going? What do you see the future of this becoming?
Cady: Right now, I definitely think we’re in our infancy. When . first came out, my providers looked at it, and they said ‘Oh, it’s a little underwhelming.’ But it has just continued and continued to grow over the last couple of months. The uses we’ve come up with — I’ve covered a couple that we didn’t even think we’d use it for. In the future, as we move to the value-based care and HCC coding, this gives us such a better-rounded view, instead of leaving unspecified, we can see exactly what the specialist coded, and make sure we’re coding to the highest specificity. There are going to be a lot of intangible benefits.
Saal: So, you’re talking possibly being able to become more effective with hierarchical coding, being able to do RAF scores a little bit differently —
Cady: More complete coding. We may not know that they’re encountering that at another specialist, and then this educates us not only in better patient care but then also better coding.
Saal: There really is an awful lot that is out there that is coming down the pike, it’s amazing, isn’t it?
Cady: Absolutely amazing. But it’s good to have a good partner like eClinicalWorks, because you’re pushing as much of it to the point of care as possible, and that’s really what needs it. Doctors and physicians can become overwhelmed with all the information being tossed at them, papers, spreadsheets, all that, and the more we can give them at the point of care, the easier it is for them to do their job.
Saal: Well, that’s just it, too. The fact that it’s in one place, you can see it on the Note there for comparison to what you’re doing, and there’s no — you’re not scrambling for stuff, as you mentioned with going through a paper chart, etc. One of the real great things about having an Electronic Medical Record.
Cady: All my staff is looking for that little red exclamation mark to tell us there’s data available. It’s almost like an Easter egg. We’re not quite sure what’ll be there, but we know there’s some more information. So it’s been very interesting.
Saal: That’s great. Well, thank you so much for spending some time with us this afternoon. We really, really do appreciate it. And thank for you some of the insights that you — or all of the insights you’ve given us today!
Cady: You’re welcome.
Saal: I’m Brian Saal for the eCW Podcast. If you’d like to see more eCW Podcasts, please check them out on iTunes, YouTube, or my.eclinicalworks.com. Have a great day everybody. Take care.





