Leveraging Population Health
Published on Wednesday, January 18, 2017
Ed Worthington, Director of IT at Northern Physicians Organization, based in Traverse City, Michigan, joins host Brian Saal to discuss how NPO uses Population Health management tools from eClinicalWorks.
Interoperability Solutions
Published on Wednesday, January 18, 2017
eClinicalWorks is committed to providing affordable interoperability to all its customers. The eCW Podcast team invited Dave Cassel, Director of Carequality, Jitin Asnaani, Executive Director of CommonWell Health Alliance, and Tushar Malhotra, product lead for interoperability at eClinicalWorks, to outline how that goal can be met.
Customizing Your EHR
Published on Wednesday, January 18, 2017
The Electronic Health Record is now a fact of life for nearly every medical organization. The eCW Podcast team sat down with Dr. Manish Shah, from Florida’s Wesley Chapel Internal Medicine & Pediatrics, to discuss how the EHR can be customized and optimized for a given organization.
Creating One Unified Medical Record
Published on Wednesday, January 18, 2017
Host Adam Siladi discusses the eClinicalWorks Acute Care Electronic Health Record with Millie Shinn, Director of Clinical Informatics from Hamilton General Hospital, in Hamilton, Texas, and gets some tips on how an organization can develop enthusiasm for change among its providers and other staff.
Cloud-Centric Acute Care EHR
Published on Wednesday, January 18, 2017
In this episode of the eCW Podcast, host Adam Siladi speaks with Dr. Scott Michener, Chief Medical
Officer at Comanche County Memorial Hospital, about the advantages of a cloud-based
Electronic Health Record in an acute-care setting.
On Track to Better Health
Published on Wednesday, January 18, 2017
Filmed live at the eClinicalWorks National Conference, eCW Podcast host Brian Saal is joined by Dr. Jordan C. Stern, founder and Chief Medical Officer of New York City-based BlueSleep Snoring & Sleep Apnea Center. The pair discuss the importance of sleeping and sleep trackers for good health.
Granting Wishes, One Child at a Time
Published on Wednesday, January 18, 2017
The eCW Podcast team had the opportunity to speak with Arianne Philion, development manager at Give Kids the World, about how the foundation grants wishes to children who are suffering from a life-threatening illness.
“From a realistic and pragmatic standpoint, it really comes down to the mobility of your population, who your patients also being seen by, and how your crossover with other organizations falls. And then who — from a pragmatic standpoint — is the best fit for connecting to the system used by those providers.”
–Dave Cassel, Director of Carequality

Topics from this episode
Population Health
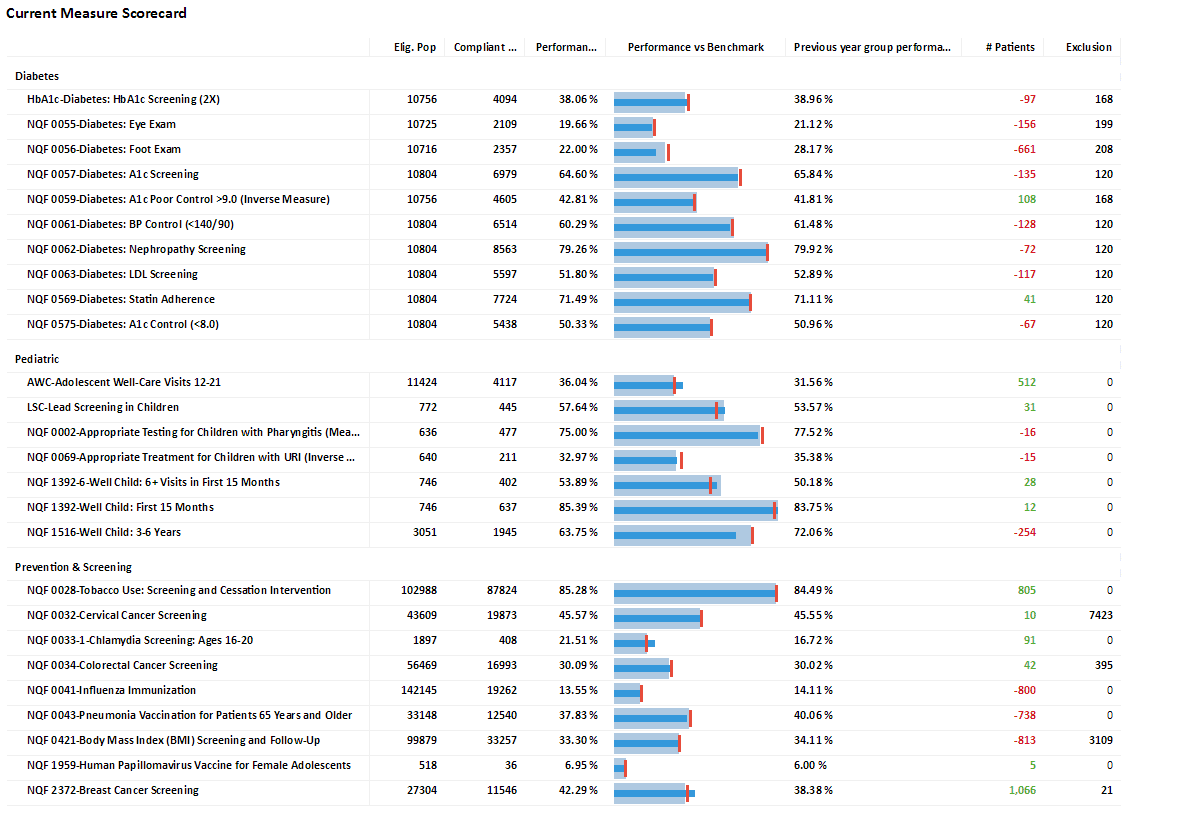
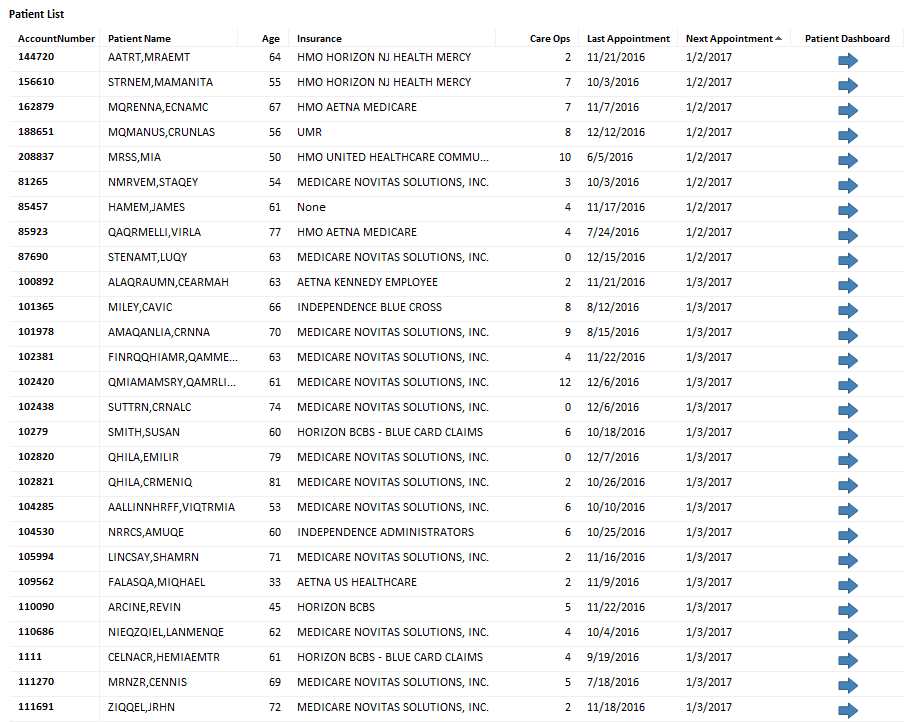
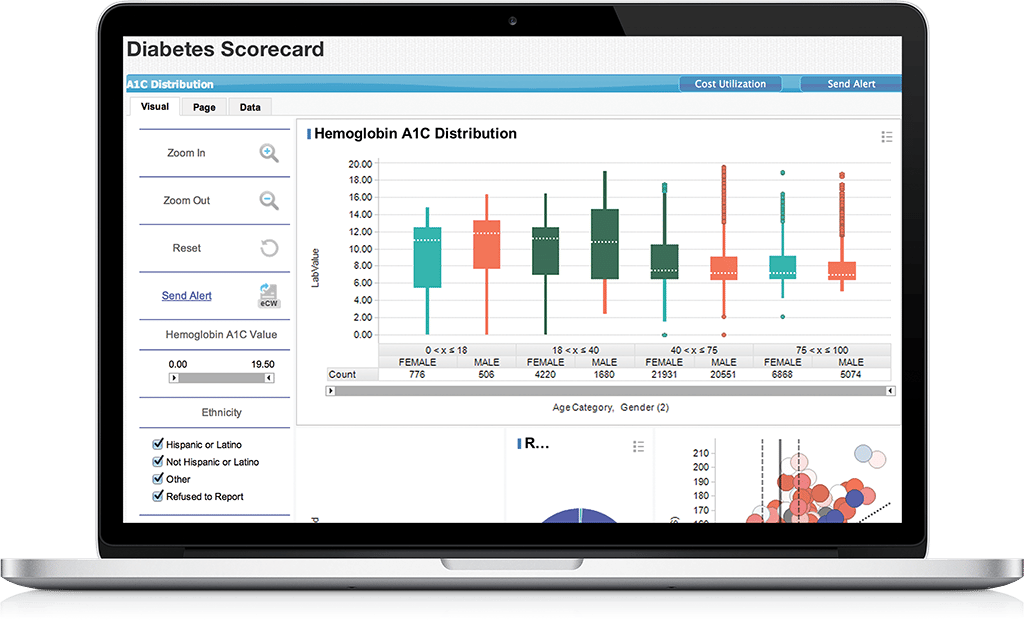
With the shift to value-based care, healthcare organizations of all kinds — private practices, clinics, health centers, ACOs, CINs, and more — are renewing their focus on Population Health.
eClinicalWorks offers a comprehensive suite of tools for improving care quality and access, identifying and closing gaps in care, deepening patient engagement, assessing risk, and meeting clinical quality measures. We also help practices with the business of healthcare, with data analytics to control costs, measure compliance, meet regulatory challengers, and achieve financial goals.
Interoperability
The eClinicalWorks interoperability platform exchanges data among many healthcare systems. Our Electronic Health eXchange (eEHX®) is a comprehensive, vendor-neutral
Health Information Exchange (HIE) solution that gives providers real-time access to a patient’s longitudinal health record at the point of care, enhancing clinical decision support, and
improving care coordination.
And eClinicalWorks is a full participant in the Carequality framework, the nation’s leader in clinical data exchange.
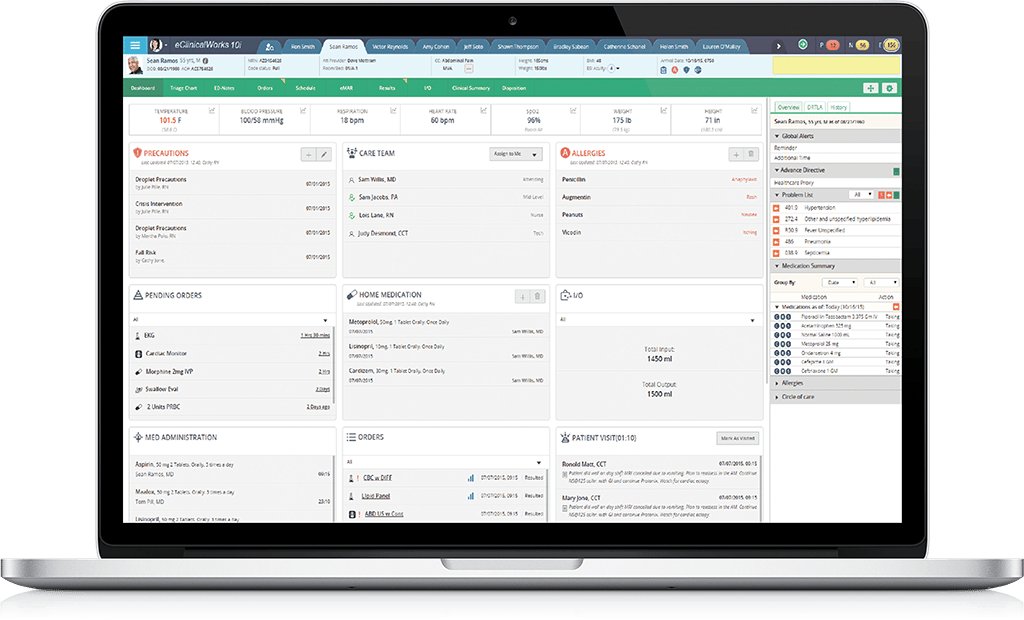
Acute Care EHR
The eClinicalWorks Acute Care EHR features a patient dashboard showing all clinical details, for Emergency Department, operating room, ICU, and inpatient units. Pharmacy and lab results are included. Organizations can manage care by census lists or floor-plan views. Documentation is accessible to all authorized users, aiding clinical decision-making and bolstering patient safety.
The Acute Care EHR creates a single medical record for your patients, eliminating the expense of multiple systems, reducing costs, and helping you remain focused on your patients.
Leveraging Population Health
Transcription:
Brian: Good afternoon and welcome to another edition of the eCW Podcast. We’re coming to you live today, from Orlando, Florida, at the eClinicalWorks National Conference and we are so happy to be here. This afternoon, I’m joined by Ed Worthington, the IT Director of the Northern Physicians Organization, or NPO. And while Ed and I were just discussing how we’re so happy we don’t have to carry pagers anymore. Today we’re going to talk a little bit about his ACO that he works for. And you’ve been an ACO for about three years, now – is that correct?
Ed: That’s correct, we’re in our third year this year and we’re been working with eClinicalWorks from the beginning, primarily with the CCMR, Population Health platform and with the eHX longitudinal record.
Brian: So, there’s a lot of data gathering and aggregation needs to be done at in an ACO – how have you leveraged CCMR to make that happen?
Ed: We have about 30 to 35 or so independent eClinicalWorks practices, in addition to quite a few non-eClinicalWorks practices. Since we’re not one big enterprise system, we needed a product that can aggregate measure data from different environments, and we use CCMR for that. We connect the different practices to one CCMR Portal. They see only their own patients, but then we also have the ability to report and track at a population level, and an additional benefit is that the practices are able to see their patients’ information, regardless of the practice they went to, so they can follow the quality measures across the practices.
Brian: And across the different EMRs, as well?
Ed: Yes.
Brian: That sounds like a pretty ambitious undertaking. How long did take you to get that in place?
Ed: We spent about a good year and a half, probably what you would call that more implementation phase. We had some people using it, we had some pilot practices right away. But we did spend a lot of time on QA, making sure the measures are accurate, building trust with the system, and then also working on adding features that made it more usable and welcome for users.
Brian: Those standards that you’re putting into place, how well were they accepted? A lot of times you’re going to get more pushback but in order to make this data aggregation to work, as you say, you have to have the data. So, did you get pushback? Or was it generally accepted across the board?
Ed: We got some pushback, in certain areas. It was actually pretty specific – certain types of documentation, certain types of documenting a certain way, not in the general goal of “We need to get towards more standardized documentation, so we can measure this on your behalf.” Really, over time we made the case, we worked with practices, maybe it’s something they gradually work into, not something they do right away, but really over the course of a year, year and a half, and we pretty much have everyone that’s on board and connected.
Brian: That’s fantastic. So, successes that you’ve had along the way, have you had any hurdles that you’ve had to overcome?
Ed: Making sure people trusted the system. A lot of the times we started, it was very early on, and we honestly had a lot we had to work through. We were just getting into this ACO business ourselves, we had to learn it and learn how to effectively measure the clinical data with them. So building a product that was usable for them, involved a lot of learning on our end, a lot of communication with them, and you know, we made mistakes along the way. You know, QA, having to spend more time on that, really listening to feedback, taking out stuff that they’re not going to use, adding in tools and features, tabs on the dashboard that they will use, and really continuing to keep people engaged and getting them to want to use it is probably the biggest challenge. Once you get past certain IT hurdles, the challenges are on the users’ side, not on the IT side.
Brian: HIE. Have you leveraged HIEs as well?
Ed: Yeah, we’re one of the 10 or 15 Health Information Exchanges in our state, Michigan, and so we use our connection to the state environment to receive admit/discharge for information, and on our end we turn those into Direct trust messages, and we email them and we send discharge information directly to the practice. We do some aggregation on our end, so they know how many times the patient has been to the ER or inpatient over six months to a year. We primarily use the HIE for ADT information and now we’re starting to on receiving those continuity of care documents for a patient’s discharge.
Brian: Oh yeah, the continuity of care documents have become very important. Within your discharges, what do you provide? Do you just give a med summary and then the regular discharge?
Ed: When we’re getting the CCDAs, in the testing phase, I’d say, in our state, about 60% or 70% of the beds, hospitals representing 60% or 70% of the beds are sending them. We get pretty much the inpatient EMR’s CCDA at discharge, so at the moment of discharge, give or take a few hours, we get exactly what EPIC would produce for CCDA, what Cerner, Meditech would produce, and we send that along through Direct. So some practices are getting them in their P2P inbox.
Brian: Can we talk a little bit about shared savings? Any success that you’ve had with that?
Ed: We saved enough in 2014, our first year, we didn’t meet the benchmark to receive money back. We saved up a million or a million and a half, and we stayed right around that mark, this year or last year and went slightly over on our benchmark and so this year we’re taking some time back and trying to reevaluate how we can really make the improvement to meet the threshold to achieve actual income back.
Brian: That’s great because it sounds like you’ve had successes not only on the patient side, but also on the remuneration side, as well. So a win/win for the organization. If you were talking to an organization that was just beginning to pull an ACO together, I mean right now, with MACRA and the final rule just being released last week, a lot of organizations or a lot of practices are going to be given a lot of different options on how they want to pursue the different tracks and trails that they can go down, whether its APMs or just going straight MIPS, and of course ACOs fall into those areas. What tips and tricks would you say or, even better, what do they need to avoid?
Ed: I think, if anyone, speaking from the IT side, if everyone’s kind of entering that area now, the one thing that they want to look it, is what are they trying to look at? What are they trying to measure, what are they trying to track, what workflows come into effect, rather than what product and then trying to find the workflow around it. I see a lot of my colleagues in other organizations their byproduct has a lot of bells and whistles, or advertised they have a lot of bells and whistles, and then they go to implement it and it’s so convoluted and it’s not usable for the people, nobody wants to get in there, it’s slow, etc. I think getting it whittled down to “This is exactly what I want to do with it. These are the exact goals that we want technology to do for us,” and then find the best solution for that. That’s where we had a lot of success.
Brian: And that’s and interesting way to come at the purchase of software, rather than look for the flashiest model, look for the model that suits your needs and then go with that.
Ed: Right, I mean I think anyone that’s worked in IT for a period of time has had the situations where you thought something was cool or interesting, and then you go show it to somebody like “We would never use that.”
Brian: Those features are fantastic but they really don’t do anything you need them to do.
Ed: And it takes up my screen so …
Brian: Exactly. Thanks so much for being with us this afternoon, I really appreciate you being here. For the eCW Podcast team, this is Brian Saal. Don’t forget to take a look at our other podcasts, you can find them on YouTube, iTunes, and my.eclinicalworks.com. Thanks for watching.
Interoperability Solutions
Transcription:
Adam: Welcome to this edition of the eClinicalWorks Podcast broadcasting to you from the eClinicalWorks National Conference in Orlando, Florida, 2016. I’m Adam Siladi and joining me today are Dave Cassel, Director of Carequality, Jitin Asnaani, Executive Director of CommonWell, and Tushar Malhotra, product lead for interoperability at eClinicalWorks. And today we’re going to be discussing the rise of interoperability, this new buzzword that’s becoming more prevalent as the industry changes. Guys, thanks for being here today and we’re looking forward to getting an idea of what this means for clients in general. Interoperability, let’s start off with kind of a contextual question, because interoperability sounds very technical, it sounds very non-medical, and I think some doctors may question “What does that mean to me and why do I need to pay attention to it?’ How would you describe interoperability to a medical professional?
Dave: Well, thanks for the question. I would describe it in a way that it is perhaps a little bit more generalized than it often is described. I see it as a means for two different systems to be able to provide information, healthcare information in this context obviously, to another system and its users in a usable way. Sometimes I’ve heard it described in an actionable way – I think it’s important to describe it in a usable way, because there are specific connotations around actual that people in the industry have made. So, in other words, as a basic provider, it’s allowing me to see information from another system that another system has packaged up and sent to me. There are, obviously, deeper levels of interoperability, where I can do things like file allergies and file medications from other systems into my local chart. But ultimately it’s about getting that information in some usable way, between two different systems.
Adam: So let’s give everyone an idea of what your two companies do, with that definition in mind. What role do each of your companies play in interoperability?
Jitin: Sure, I’ll go ahead and take a stab first. So, CommonWell Health Alliance is a not-for-profit organization focused on enabling the patient’s data to follow the patient regardless of where their care occurs. So the intention is that wherever physician or any other sort caregiver is taking care of a patient, they should be able to access that patient’s data across our network. So we built this network that enables thousands of endpoints to be able to share that data are able to share that data centered around that specific patient.
Dave: And from the Carequality perspective, we’re involved in ultimately a very similar goal, but we approach it a different way, and I think our mission really is complementary to the one that Commonwell has. As Jitin described their efforts of building a network, there are others who have also built networks, whether those are vendor-based, whether those are regionally based, and in general we don’t refer to them as much as networks, as really communities that have come together, the network is secondary, but the communities have come together to meet their data-sharing and interoperability needs, and networks and other programs have developed out of that. Historically, and this is certainly no commentary on CommonWell specifically, it’s just historically the case for all of these data-sharing networks, they haven’t allowed folks to connect in a systematic way, between and among the networks. So, it’s a little bit like having a cellphone from Verizon and only being able to call other Verizon customers. What Carequality’s mission is, is to provide the framework for all of these different data sharing networks to connect their clients and their members to one another – so that you can cross, not only the EHR vendor and other platform boundaries, but also crossing the network boundaries, very much like what the software industry has done to connect various cellphone networks together.
Adam: There’s a couple concepts that are coming up here. You mentioned the information following the patient, that seems very similar for what CMS is going to ask people to start doing when they’re monitoring their cost component, especially of MIPS and MACRA. So, doctors have wondered “How am I supposed to be able to see what is going on with my patient across all of these settings of care, and you look like you’re trying to provide that information. And then, Dave, to what you said, it sounds like this is a common theme for technology. As the fax machine, that’s become such a backbone to so many organizations, became more powerful the more faxes were online. Computers became more powerful the more systems connected to the internet. It sounds like the EHR is going to become more powerful the more networks integrate, these health communities integrate with each other. So it sounds like there’s a lot of benefit for everyone – for providers, for patients, to large organizations, but which offices might want to sign up sooner rather than later for something like this?
Dave: Well, I consider prioritization, I think ultimately we would think that the work that we’re doing is valuable to any physician and any practice. From a realistic and pragmatic prioritization standpoint, I think it really comes down to the mobility of your population and who were your patients are also being seen by, how your crossover with other organizations falls. And then who, from a pragmatic standpoint, who the best fit is for connecting to the system used by those providers, and I don’t know if you guys want to add your perspective, as well?
Jitin: Yeah, I’ll absolutely agree, and I’ll add on as well that it is – the mobility of the patient definitely has a great impact, but it’s also – actually building on David’s point — it’s also the diversity of care locations where the patient goes for healthand care purposes. If you think about it, in any healthcare community, in any community really, across the US, have, with things like clinics, you have things like hospitals, those are your traditional healthcare places, but there are also a variety of other settings to which patients go for care; portals of their own, apps, tools that they may use. Homecare settings, nursing facilities – those are the types of places especially now that we have an aging population that are more and more relevant to health and care. Imaging centers, dialysis centers – such a broad spectrum of different places patients may go. One interesting thing about CommonWell and also Carequality is that we’re not limited to just EHRs. EHRs are a huge part of our network, but we’re really about insuring wherever that patient goes for care that their data is available to those providing care to them.
Adam: How does something like this, and when we’re talking about interoperability, a couple of concepts have come before, so providers might wonder, “Well, I’ve already tried to get onto that one, why do I need this one?’ So Direct comes to mind, that was a big push of recently, especially with Meaningful Use, how does this compare to Direct?
Tushar: So, it’s essentially a different use case, that’s how I look at it. The doctors are trying to send referrals from, let’s say, a PCP to a specialist, that’s where Direct can help. But this is an entirely different use case. Regardless of where the patient has been given care at, you can query the data. As Jitin was just mentioning, it could be a lab company, it could be radiology, it doesn’t have to be an EHR, there could be data sitting in an HIE depository for that patient. We will fetch that data using a query mechanism and pull it at the EHR level and display it to the provider, and make it meaningful so that they can see it in a consolidated way.
Adam: So it sounds like, maybe with Direct, you were somewhat reliant on the person on the other side to send you the information, but these networks maybe make you a little bit more self-reliant because you can go find the information when you need it. Another buzzword that was going around for a while is HIE, the Health Information Exchange. How might this be different than that scenario, as well?
JItin: Sure, so an HIE, capital H, capital I, capital E, Health Information Exchange, it’s really, first a couple things, activity is data sharing and in many ways this is not that different, but the organizations with HIE are typically set up more around regions, communities, etc. They meaningfully serve those communities and those areas or populations that they serve. What CommonWell is, is a national network, so there’s no boundaries beyond the US – it’s wherever a patient goes within the US, the intention is that that data is available, and that creates a national fabric for healthcare data exchanges and particularly for query and retrieve which is our current use case. That allows us to enable HIEs, EHRs, other types of health IT systems to be able to plug in and utilize. So it really is less of a conflict and much more of just a different type of use case that enables a number of different types of organizations to be able to connect and utilize the same sort of services.
Tushar: To add to that, in our experience, what we have seen in the past is that HIEs would typically be aggregation of data – this is very decentralized. It could be multiple repositories that you are querying and fetching the data for the provider, and you don’t have to log into a second portal to view the data, it’s all at the point of care, and that’s where the biggest value is.
Dave: Just to give the Carequality perspective there on the HIE question. From our standpoint, and I mentioned earlier the concept of communities coming together, not all of those are certainly regionally based but some are, and they form these Health Information Exchanges. From Carequality standpoint, that’s just one other type of network or data-sharing program that we would see connecting underneath our framework – still providing a lot of value, whether that’s around the aggregation services, notifications, other types of things, but for the core use cases, where there is a need to communicate with our members of other efforts, other networks, they would be able to do that via the Carequality framework.
Adam: Now we’re two different solutions, very closely related, why might a doctor or an office need both? I’m assuming they want to be on both, there’s some benefit there?
Dave: Sure, I’ll take a first stab at that, and certainly interested in Jitin’s perspective on this, as well. From my standpoint, it comes down to you do want both in all likelihoods, for different reasons. The CommonWell platform offers a number of core services to its network members, and if you’re taking advantage of those services, which go above and beyond what you would do with Carequality, that is sort of its own use case and you would evaluate those services. To the extent that you also want to have the capability of exchanging in this very broad ecosystem of different data sharing networks that Careqaulity enables, being able to query into your local Epic hospital, for example, or allowing connected patients to via their PHR provider to come in and get your records, or even accessing records for a health plan for care coordination. All of those things you can do through the Carequality framework via the eClinicalWorks network, via possibly an HIE that you’re already involved in. There are a number of different platforms, but all told, there are two different use cases and it’s ultimately about the services from CommonWell versus the widespread exchange capabilities from the Carequality framework.
Jitin: I’ll add into that. I agree. As CommonWell focuses on that individual and insuring that individual’s data goes everywhere, we have a set of services that will continue to expand, that will allow providers to be able to exchange that data around that patient in more and more valuable ways that fit into the clinical job that the provider is trying to accomplish. That’s why we have the domain in which we will continue staying whereas there’s a wide variety of other very legitimate valuable interoperability use cases. Interoperability is a very broad and deep environment, and in that case you are also looking to be able to participate in those types of information sharing networks. So I think you’ll want to be part of not just CommonWell and Carequality, but all those other types of organizations and exchanges that are meaningful to your organization and your goals. The one other thing I’ll add is, at least in the short term, hopefully not in the long term but in the short term, as our organizations have sprung up only in the last couple of years and Direct project itself, being the grandfather of all of this is only like four years old, really. We’re talking about many of our community members, EHR vendors, for example, but not just EHR vendors, who are participating in one place or the other, and in the short term it makes a lot of sense for everybody to try to participate in a few different places because that gives you better coverage of your patients, no matter where they go. Over time, obviously, we hope that will all converge and it’ll really just be about what is the value you’re trying to extract at that moment.
Tushar: And just to simplify it, like, in the shortest term, right now, the most value that a practice can get is by connecting to Carequality, is by getting connected to the local Epic hospital, and the Cerner hospitals through CommonWell, and that, I think is the biggest value piece in the shortest term, I would say, right now. Things of course can change, there could be participation from both vendors, from both networks, in both frameworks, but as of now, that’s the biggest value add, which is probably like 50% of the inpatient market space that these two vendors have. I think that’s a big –
Adam: I’m sorry, I’m just going to have to cut you short there because we’re running short on time. The big important question that we want answered, here, at this moment, is now what does this mean for the user? What does the doctor see when they go to leverage this stuff in eClinicalWorks?
Tushar: In the end, it’s the data that they are able to see from the Epic hospital or the Cerner hospital, or any other ambulatory EMR that they are exchanging data with. So any critical exchange partner with, who is on CommonWell or Carequality, we will fetch the data, put it in the Right Chart Panel of the Progress Note, make it discretely importable like allergies, medications, problem lists. Give them an opportunity to view the complete CCDA or any other information could be packaged inside a PDF – that’s what they can view in the EHR.
Adam: Excellent, so like I said we’re just about out of time here, but before we go, I’d like to ask if clients have any questions here at the conference, where can they go to get some more information? Or even afterwards?
Tushar: So, myself and our team are at the interoperability booth in eCW Central, these guys are here through today, and they can answer some question, as well. In addition to that, we can always be reached at interop@eclinicalworks.com for any questions about this.
Adam: Wonderful. Well, guys, thank you so much and we’re going to, like I said we’re out of time, we’re going to have to wrap up, but I think this has been a wonderful conversation, thanks for all of your input. Dave, Jitin, Tushar, thank you for being here today. For the eClinicalWorks podcast, I’m Adam Siladi. You can check out our other podcasts on iTunes, YouTube, and my.eclinicalworks.com. Thanks for watching.
Customization of the System
Adam: Hello and welcome to this edition to the eClinicalWorks Podcast, broadcasting from the eClinicalWorks National Conference in Orlando, Florida, 2016. eClinicalWorks is often touted as a very flexible system with a lot of customizable activity, capabilities I should say, and here to speak with me about that is morning is Dr. Manish Shah MD, internist and pediatrician from Tampa, Florida, Dr. Shah, thanks for being here today.
Dr. Shah: Oh, no problem. Thank you for having me.
Adam: Now, we’re talking about customization of the system, and you had a very unique use case for that. You have an office in Tampa, Florida, but you said that you, all of a sudden, one day had to start worrying about Zika – what a very timely topic. Tell us about that.
Dr. Shah: Sure, we had a patient that traveled on a cruise to the Caribbean, and she came back with symptoms consistent with Zika – fever and joint aches. She immediately looked up herself, if this was something that could be related to the Zika virus. At that point in time, she said “Well, maybe I need to come in and get checked out.” At that point in time, she came to my office and we had some interesting conversations and then led to us wanting to test her for the Zika virus.
Adam: So this scenario is obviously one that’s just recently started becoming an issue in this country. So I had to ask the question, did your lab compendium have the test that you needed to figure that out?
Dr. Shah: Right, so at the time, it was about two months ago, none of the labs had completely set up their Zika virus testing – however, LabCorp and Quest had come out with their testing, but it couldn’t have been pushed to the compendium right away. So they weren’t in the compendium so we had to go in and add them into the system.
Adam: and you were able to do that through your EMR labs menu, tell us about that process.
Dr. Shah: Correct, so when you go into the labs menu, and you go to lab diagnosis procedures, you can add in testing, as long as you have a CPT code. So going into the Quest test center of the LabCorp menu, you can go in, search ‘Zika Virus,’ find those tests, and then put in the CPT codes and then make a new code or make a new test. Once you’ve added that test into the menu, then you can go about ordering it, which made it much easier for us because we went ahead and did that, and we were able to communicate what tests we wanted to them, which went through successfully.
Adam: So you didn’t have to wait around for some outside source to push the information to you, which might have taken months, you were able to go in, configure those labs, set up all of the correct lab codes and link codes in association so you can broadcast that through your lab interface so you can get that to the lab company in the correct manner so they can get you the information back.
Dr. Shah: Correct, one you can get a test code from their website, so, typically, going to questdiagnostics.com or labcorp.com, looking up their test menus is very, pretty reasonable, so typing in Zika is not going to give you a bunch of results, so it was pretty straight forward to find their test codes. Then, adding them in, as long as you have the correct test codes in, made a transfer.
Adam: So how did that go? Were you able to perform the test, do the draw, and get the results you were looking for?
Dr. Shah: So, I hesitate with this answer which is, unfortunately, because there are specific requirements for the specimens, including refrigerating specimens for Quest, or freezing the specimen for LabCorp, we were not able to get it there correctly. They had some new processes, that were required by the CDC, which required that the samples be completely separate from other testing, and when you order Zika testing, you should also be doing some dengue virus testing antibodies, and unfortunately if you just send one file, they can only do the dengue virus testing, so we were not able to get the Zika testing, as well.
Adam: So there are some additional pieces of information that we might not be used to seeing, maybe there are some specific questions in that case and in eClinicalWorks can allow you to configure those things, as well.
Dr. Shah: Absolutely, so the “ask and order” entry feature in eClinicalWorks is very helpful there because then you can notify the lab while you’re testing a patient, because one of the requirements, at that time, was that the patient should be pregnant and that we document what symptoms they had and a travel history which, at that point, would give the lab the information that they need to proceed with the testing without having to call you to verify the need for that testing.
Adam: Now, the question will of course become: well how do we effectively get that information? eClinicalWorks obviously provides some tools for that, which we’ll discuss in a little bit. But once we’ve configured those pop-up pieces of information, which, of course, patient safety comes into play there, which is the topic of everybody’s mind today, what information do we maybe need to start conveying to patients regarding these scenarios?
Dr. Shah: I think, in general, for Zika, anybody that has a travel history to the Caribbean or South America, they should be tested if they’re pregnant. For people that are not pregnant, the symptoms could initiate testing, so if you have a fever and joint aches, then those people should be tested. I think the nice thing about eClinicalWorks is that we have a whole bunch of different options that we can use to capture those patients that would actually need testing and would benefit from testing, by either using the Messenger or something with the Kiosk, adding a questionnaire in the Kiosk, if you’re using the Kiosk, sending out a message through the Messenger, or even Portal messages for your patients that it would apply to.
Adam: Right, certainly a lot of very important information that we want to maybe broadcast to a large set of our patients. If we had to try to do that through the phone or wait for them to come in, that just wouldn’t work for us. Obviously eClinicalWorks provides eClinical Messenger, which you can use to call or text your patients with certain messages or information that they should come in, and then there’s also publishing messages to the Patient Portal if you’ve been getting them on there. Now, the other thing is you mentioned that we want to ask them that specific questions, and I want to mention that the eClinicalWorks Patient Portal gives you the ability to publish a questionnaire to the Portal, so that you can send the patients a message, saying this questionnaire is available, we would like you to fill it out. They can log into their Portal and answer those specific questions, and of course that information will flow to your EMR, so that you can take action on it, follow-up action. And you mentioned another place you might capture that action, as well.
Dr. Shah: I think the Kiosk, on check-in, would be huge, because if they didn’t answer it in the Portal, at least you have the other option of catching them when they’re actually in their office. It’s always frustrating when the patient is in the office and you’re like “Oh, I forgot about the flu shot or the pneumonia vaccine,” and if you have that question already there, the next thing you know. So at least it’s populating for you, you know that, that person has an actionable result you need to take care of, which is huge because it takes that little bit of load off of you to take care of all their other problems that you’re commonly dealing with.
Adam: Right, using that iPad Kiosk that eClinicalWorks supports, you can put a questionnaire item in there as well, so when the patient checks in, we’re sure that we’re going to answer that item. Great usage of that technology there. Now, we’re in Florida, and Florida’s known for being a place where there’s a lot of older patients. In the care that you deliver, do you find that older patients are less likely to use the Patient Portal?
Dr. Shah: Actually, my experience is exactly the opposite. My older patients aren’t afraid of the Kiosk at all. They’re not afraid of using their computers. Most of them are calling me when they’re results aren’t on the system soon enough. For the most part, they’re actually very computer savvy. There are a few people, and I’d say a very small number of people that tend to avoid the computer, but for the most part, they’re logging on in the Portal, they’re asking to get their logins reset, so I know they’re using them, and our population is at least 20% over 65, and our utilization rate for the portal is, I would suspect, 75% or higher.
Adam: Those certainly sound like some very successful numbers there, so, of course, that leads to the second question – the first anxiety that people have is “Well, what’s the use of getting patients on the Portal, especially those older ones, they might not even use it.?” You’ve said that that’s not the case, that they’re willing to use it. Now, the next question that people have is the next hesitation that they encounter is that, “Well now, am I going to be bombarded with messages, is my whole day going to be taken up with secure messaging?” Does this secure messaging through the portal make your job easier or harder?
Dr. Shah: Often times it makes it easier, I have my patients, instead of calling the office, use the Portal to communicate directly with me – if I need them to call me back with their blood pressure or their blood sugars, they’re using the Portal to tell me that their blood pressures are actually fine, or their blood sugars are fine or, if they’re not, I can make an adjustment on the flight, and not have to have them come back for another visit, which, when you’ve just seen them a couple of days ago and you’ve told them “Hey, your blood sugars are not better, I need you to do this,” that documents it cleaner and I think, when we’re documenting cleaner, at least you know, going back I just did this, and this is what I was going to do, and I’ve documented now what I’m planning to do.
Adam: So flexibility, organization, cleaning up workflows, simplifying things for you and other doctors.
Dr. Shah: Absolutely, and I think the documentation is even more key because now you’ve actually seen what you were thinking all along because if you may have had a phone conversation and didn’t document it, I think that’s a little bit of a guessing game later – “What did I tell you to do?” or “What are you doing now?” I think having it documented is so much cleaner, and that messaging function makes it that much cleaner because you’re directly communicating with the patient, especially for your complicated patients.
Adam: Well Dr. Shah, thank you so much for sharing your thoughts with us, thank you for being here at our National Conference.
Dr. Shah: I appreciate you having me.
Adam: And we’re going to sign off now, but thanks for watching this episode of the eClinicalWorks Podcast. You can check out our other episodes on iTunes, YouTube, and my.eclinicalworks.com. For the eClinicalWorks podcast, I’m Adam Siladi – thanks for watching.
The Acute Care EHR
Transcription:
Adam: Welcome to this edition of the eClinicalWorks Podcast, I’m Adam Siladi and we’re broadcasting from the eClinicalWorks National Conference 2016 in Orlando, Florida. eClinicalWorks has been a longtime leader in the ambulatory EHR space, but we’re not developing offerings to be used specifically in an acute care setting, and we bring our technical expertise to partner with some people with the clinical and procedure expertise. And that’s why Millie Shinn is here with me today to discuss that. Millie, thanks for being here today.
Millie: Thank you for having me.
Adam: Now, Millie, you’re the director of clinical informatics at Hamilton County Hospital in Texas. Tell us a little bit about your organization.
Millie: So, we are a hospital-based RHC, we have three clinics that span in three different locations. There’s 12 providers total. We’re also a 42-bed PPS hospital, so we’re one of the smaller hospitals, but still not critical access.
Adam: 10i, new product, obviously, and you are our development partner, and that is not something that just anybody gets to be a part of. Tell us a little bit about how you came to find yourself involved with it.
Millie: Yeah, I think we had this discussion earlier. I’m a little pushy, so we ended up going to the conference last year, they made the big announcement. Girish said that there was going to be an inpatient product. There was about three or four of us there from our facility and we decided that that would be game changing for us, a unified EMR. So I went down to the 10i booth, skipped a session, but it was OK. I met Roneil, Roneil’s the lead developer for the product, and I asked him to show it to me. I watched it, it looked great, there were a few things that we could improve, and so I gave him just a little bit of feedback right away. And went back and talked to all of my coworkers, and we kind of brainstormed how would this affect us, how would this affect our users, we decided we want to look at it again. So I went back the second day, and I looked at it again. And a third day, and by the third day, Roneil and I had kind of built a rapport. He brought Girish in, and we talked – Girish and I and Dr. Rudolph, one of our doctors, agreed that this is something we want to move forward with. So they sent us a letter to commit to the project.
Adam: Well it doesn’t sound like you were being pushy, it sounds like you were being helpful, so I wouldn’t say pushy. I heard you are also the leader of a Google User Group.
Millie: I am, I have a Google User Group – it’s currently our existing vendor, but we’re opening those up. There’s about 270 users that are all clinical in background, so you may have a pharmacist, a lab director, informatics people like myself. So it’s really kind of throwing ideas around the healthcare IT pain points and how other people are solving those problems.
Adam: Let’s talk about some of those pain points. With your current configuration, your current setup, what are some of the pain points that you face?
Millie: So we have three EMRs, we have one in our ED, one in our three clinics, and one in our inpatient system. So when you’ve got three EMRs, you’ve got three usernames and password, you’ve got the patient’s home medication list that has to be re-entered three times, so you lack that ability to really create a seamless experience for the user or the patient. So we felt like those were things that really mattered to us.
Adam: And that’s not an uncommon situation especially in a hospital setting, you’ve got lots of different systems designed for different things, that probably came online at different times and now you’re trying to get them all online to talk to each other. It also sounds like there’s some patient safety issues going on there, when you have to duplicate the information across multiple systems, one of them might get missed, or entered incorrectly. So how do you think that 10i will solve some of these problems?
Millie: It changes everything. I think that, for us, the ability for the end-user experience, when they’ve got one system and all of the information is at their fingertips, regardless of where they work, it’s the same system so they can access that information from anywhere. I think that, as a nurse, to me, the med list, entering it once, and not having to duplicate that process is safer for my patients and it’s easier for me. And then upon discharge it will be readily available to the next clinic visit, so that information is already there waiting on us.
Adam: Why do you think people don’t have that unified system already?
Millie: Cost. I mean, we’re a small hospital, so cost is everything to us. And in the past, the unified EMRs like Epic and Cerner, those are expensive – they’re not cost effective for a small facility. So last year when Girish said that he really wanted to kind of disrupt the market, and after something that was scalable, I mean, we should never have to sacrifice our patients safety or experience or our end-user experience just because we can’t afford it. That was something that Girish committed to then, that he wanted to offer something that everyone can afford and give their patients the exact same offering.
Adam: Are there any functions or modules or anything like that, that you might have been working on, that you know are distinctly different from the ambulatory to the acute care setting – messaging, for example, or anything like that?
Millie: So one of the things that we kind of talked with eCW about is that, whenever you’re in the ambulatory setting, someone’s sitting behind a desk, or they’re on their iPad, pretty commonly, frequently, but for the inpatient setting, we’re down in patient rooms – we’re not sitting in front of a desktop, we’re not sitting in front of an iPad. So whenever you want to communicate with physicians, or a patient family, or anything like that, you need to be able to push that information out. So we think the ability to send someone a text, a secure texting app, or something that will send that information to the doctor and alert them to where they’re like OK, I have the information I need to handle, and I think that’s something that we’re really looking forward to changing for us.
Adam: And certainly we’re seen some pretty cool features coming out with regards to messaging, from everything, not just the clinical members that you’re talking about, but also in the inpatient setting, you have housekeeping, transportation, bed management, that kind of thing, and then messaging can communicate with all of those parties in a unified way. So let’s talk about this development process – you had a close contact with Roneil on the development team, but what about looping in some of the other people in your organization. What kind of information and feedback have you gotten?
Millie: We made a concerted effort that these are the people, we’re engaged all of our directors, so the lab module is being developed by our lab director. We have made sure that these people were engaged at the beginning levels because when this transition happens and we want to change over, we make sure that they were engaged in the process. So we’re had all of our directors involved from the very beginning. We meet monthly and talk about how things are going in the project, how they’re feeling. I sent out a survey about a month ago, because we’re almost a year in now, and so I sent out a survey to make sure they’re still feeling OK with the project. I sent out to 22 directors, we’re pretty small, I sent it out to 22 people, and I got 19 back. One of the questions was “Is this making your life easier or harder or are you indifferent?” All of them across the board said “Easier.” As far as how excited they were to make the transition into the new product, five was super-psyched and zero was not at all, and I had all but two were super-psyched, and they were all four – like it’s zero to five, and they were fours, so I was like “OK, close!”
Adam: That sounds like a very excited group of people. Now when we come to implementation, still a ways down the road, but especially something like an acute care setting, we have a lot of different parties involved, and a lot of people – it’s a big undertaking, right? I’m sure it causes some anxiety. How do you plan to roll out that implementation?
Millie: You know, we have a history of when we go live with something, we go big or go home. So I think as long as we make a super-fun event, we’ll have to see what we bring to the table. I think there’s going to be some sort of a large event that will last throughout the implementation phase. We tend to throw food and gifts at them, and it makes them happy.
Adam: What are some events that you might have done in the past?
Millie: We did a NASCAR-themed event, the last time we went live. So NASCAR came in with a car that we got to ride in, and we put all of our directors, their departments were able to make them their own “race car.” So, my director, he got to wear a nice little tag and ride a tricycle that was his race car that we made for him. So it was kind of fun.
Adam: That does sound like a lot of fun. Any thoughts on what you might be planning for the next one?
Millie: I don’t know, it’s hard, we kind of topped ourselves out with NASCAR. We’ve talked about the circus, or I don’t know, we’ll have to see.
Adam: Well, it sounds like a lot of fun and maybe you can start a side business as an implementation consultant for other hospitals, how to make your implementations fun. Well, Millie, thanks so much for taking the time to speak with us today. If you’d like more information about our acute care offerings, you can go to my.eclinicalworks.com, and you can also check out our other episodes on the eClinicalWorks podcast on YouTube, iTunes, or my.eclinicalworks.com, as well. For the eClinicalWorks Podcast, I’m Adam Siladi, thanks for watching.
Cloud-Centric Acute Care EHR
Transcription:
Adam: Hello and welcome to this edition of the eClinicalWorks Podcast, I’m Adam Siladi and we’re broadcasting from the eClinicalWorks National Conference in Orlando, Florida. With me today is Dr. Scott Michener, CMO and practicing urologist at Comanche County Memorial Hospital – welcome to the show.
Dr. Michener: Thanks for having me.
Adam: eClinicalWorks, as we’ve seen from this conference and the keynote that Girish gave, is always trying to be at the forefront of technology, always trying to offer new things, and that has led us to some collaborative relationships in the development of our 10i acute care module, and you have a lot of experience with that, as one of our collaborative partners, don’t you?
Dr. Michener: I do.
Adam: So tell us a little bit about the hospital and your group.
Dr. Michener: We’re a 240-bed community hospital in Southwest Oklahoma, non-profit, we have about 270 physicians on staff, we have 100 men employed, a physician group, multi-specialty, we do a level 3 trauma, cardiac, neurosurgery, kind of a basic regular, good ol’ American community hospital.
Adam: And we’ve been working very closely with you to develop that 10i system and improve the offerings there. Tell me how you got to be involved with that collaborative relationship.
Dr. Michener: Well we came to eCW on the outpatient side in 2011. At that time, I met Jinesh Gandhi, one of the people in sales at the time. We took our group live in either late 2011 or late 2012. Jinesh and I became friends over the years, and kept in touch. He would often check on me, and through these conferences we just kind of kept in touch. He told me about two years ago, that they’re going to start working on a hospital system. We had some interest in it, then, and over the years had been communicating about it. Last year at this conference, we saw a brief demo on that that took off from there. At the end of ’15 we became a collaborative partner on the 10i project.
Adam: Wonderful. So what has that collaborative relationship been like? What’s it been like to work closely with the developers and the team?
Dr. Michener: Well, eCW’s really treated us as a partner, it’s been a partnership. We’ve had a team from eCW at our facility every week probably for the last year working on all aspects. Basically, it was a real open relationship, we just kind of opened the doors to the hospital and gave them access to all our experts in various areas. They’ve had us to Boston, we’ve had some of our nurses to Boston, and it’s been a real work in progress. We’ve seen things, our suggestions that have come to fruition in the medical record, the engineers solve our pain points, it’s been real nice.
Adam: So when we’re talking about your Go Live, what do you think that will look like? I mean it’s a large undertaking, a lot of developing going on – are you planning to phase this in or is it going to happen all at once?
Dr. Michener: Well, we’ve talked about that a lot, there’s pros and cons to both. We are live on a system now, and I feel likethat living in two different systems, isn’t probably best on the patient and it’s hard on the nurses, hard on the staff. So our plan, in phase one, is to take all the big areas up in the first phase – that’ll be ER, med/surg, labor and delivery, recovery. So essentially we’ll do is kind of a big bang and bring everything up all at one time.
Adam: Well, I’m sure in a setting like acute care setting, there’s so many different things that interact, so you probably have to do it all together.
Dr. Michener: Yes, this is pharmacy, it’s lab, it’s surgery, it’s labor and delivery, it’s allied health, RT, PT, nursing, it’s ER. It’s a big undertaking.
Adam: Obviously there’s a reason for change, a reason for change to try to improve what our experience is. What are some of the pain points that you’re trying to resolve, by moving to an eClinicalWorks integrated acute care system?
Dr. Michener: Well, for our community, we’re a big system, and we have five different EMRs, and not one of the different EMRs talk. We have an in-patient EMR, we have a cancer EMR at our cancer center, we have eClinicalWorks in a big multi-specialty group, and there’s no communication between the two and there’s no communication between the physicians and the hospital. So, really, our biggest goal is to have one unified record, we’ll be on one platform, there will be one health record for the patient, so that it will be a continuum of care from the out-patient to the in-patient to the rehab – to wherever our patients go. So we’re really excited about that. The physicians will be able to see their records and share their records betters. So really the biggest paint point we’re going to fix is too many systems, bringing it down to one.
Adam: And how do you think 10i will do that? What do you think you’ll see?
Dr. Michener: Well, I can’t speak for the computer side of it, but we’re going to be one record. My outpatient record and my inpatient record is truly going to be one record, one platform. We’ve talked about with just a click of a button, you can go from the outpatient to the inpatient record. So when a patient goes from the office to the ER, the ER doc will see the record. When they leave the ER and go to surgery or the hospitalist, they’ll have their record. When they go back to their primary care, that primary care will have the hospital record. So it will truly be one unified record.
Adam: And I’m sure that will make a lot of those coordination of care measures and focuses that are becoming more and more part of the delivering care much easier, right? If you have to do a follow-up after a patient gets hospitalized, now you’ll be able to see that they were hospitalized.
Dr. Michener: You know, the possibility of scheduling and seeing that. Today, we saw one of the demonstrations we saw real-time quality metrics, where you can look at a dashboard for the day, and follow your patient in the hospital and make sure that they’re meeting the necessary best practices and quality metrics. So it’s going to be transformative for our institution, I really feel like.
Adam: Is there a role that you see for technology, in general, in terms of medical care and what you give to the patients?
Dr. Michener: You mean, besides doctors don’t like it very much?!
Adam: Well, I think one of the big catch words right now is patient safety. It was a big part of Girish’s keynote this year, at the conference. Do you think it’s going to have any kind of an effect on that?
Dr. Michener: I think our medication areas go down. You know, Dr. Raj talks about patient safety being a three-legged stool – the electronic record, the best practices or the governance of that medical technology, and then the end-user, the nurses, physicians. So we all have to work together, and that’s some of the stuff we’re doing with eCW, we’re trying to be a part of developing best practices and sharing those best practices so we can all take better care of the patients at the end of the day.
Adam: What about the feedback and the interaction between eClinicalWorks and your group during the development of this.
Dr. Michener: It’s been really an amazing process to watch. We’re healthcare providers and eClinicalWorks is a lot of engineers and engineers tend to solve problems and healthcare workers tend to take care of patients. So what we’ve done is we put some of our best people with those engineers and they just spent days with them, they spent days in surgery, they’ve spent days on the floor, they’ve spent days in PT, they’ve spent hours in the pharmacy and the lab. So, if we communicate correctly to them then they transform that into problem solving and making a record. So it’s been fun to watch, our staff has really enjoyed it because they spend that time with them and then three months later they come back and show them what they’ve created for them to make their day better and take better care of patients. So it’s been a real nice process.
Adam: Now I know this is a project that eClinicalWorks management is very invested in and excited about, and I think you had a story to share.
Dr. Michener: So, eClinical – Girish and Dr. Raj came to our community hospital to tour and to see us. I was walking with him up on the floor, we were walking on the nurses floor and up on the med/surg floor, and one of our nurse managers was walking and I introduced him, and she started right away telling him what she wanted in the medical record – ‘Hey, I forgot to tell you something, I want this, I want that, I want this.’ And Girish got a big kick out of it because he saw how motivated and how passionate she was about the change and making it better, so it was real nice.
Adam: Well, we’re certainly excited to be going on this journey with you, and we hope we get a chance to see a lot more of that coming out in the future. Now you’re also part of the patient safety panel with Dr. Raj at this year’s conference.
Dr. Michener: Which has been real nice. eCW developed a physician advisory committee for patient safety. It’s very well represented, it has a pediatrician on there, it has a geriatric physician on there, it has a very knowledgeable pharmacist on there, it has some of the 10i group, a surgeon, and so really we’re trying to help eCW through all their other partnerships, just get out the best practice and try to shoot for that goal of zero patient harm and really just do the best we can by our patients, using technology to do that.
Adam: Are there any discussions or maybe attendee questions that stood out for you from that session?
Dr. Michener: Oh, a lot. Mostly the medication reconciliation and medication management – being safer in what we prescribe, but we also talk just about a culture of safety and having it at the forefront of everything we do. It’s hard trying to take the variability out of medicine, and so we do the same thing and provide the best for our patients. And that’s hard when there’s so many variables in the game, but it’s been a good journey so far.
Adam: Well I’m sure the attendees from your panel were grateful to be able to learn from your vast experience. I think we have a panel session just about every session of today’s schedule, so be sure to check those out. If you join us for our conference next year, you can definitely learn from a lot of those. Dr. Michener, thank you so much for being here today, we want to thank you for your time and your insight. Be sure to watch our other podcast episodes on iTunes, YouTube, and on my.eclinicalworks.com. For the eClinicalWorks podcast, I’m Adam Siladi, thanks for watching.
On Track to Better Health with healow
Transcription:
Brian: Hello, and welcome to another eCW Podcast, I’m Brian Saal, and today we’re broadcasting live from the eCW National Conference here in Orlando, Florida. Joining me today is Dr. Jordan Stern from the BlueSleep Snoring & Sleep Apnea Center, founder and Chief Medical Officer in Manhattan. Thank you for being with us, today.
Dr. Stern: Thank you for inviting me, it’s my first time here.
Brian: I’m hoping you’re enjoying it.
Dr. Stern: Very much.
Brian: I wanted to talk to you a little bit today about the new advent of wearable medical devices. We know about FitBits and so forth, but before we do that, can you tell us a little bit about your practice?
Dr. Stern: So the BlueSleep practice in New York City is a practice dedicated to the diagnosis and treatment of sleep apnea and other sleep disorders, with an interest in technology and new technology and making it as easy as possible for patients and their families to be diagnosed and treated. So we’ve been using home sleep testing technology for about 15 years, we’ve done over 10,000 home sleep tests — much easier to get a study in your own home, also 10% of the cost of a sleep study — and we’ve also very interested in wearable technology and sensors and how they can play a role in increasing the number of people that are undiagnosed that do have sleep apnea. Probably in the United States, we’re looking at 50 to 100 million Americans that have sleep apnea, and 90% of those are undiagnosed. So, all about making it easy for diagnosis on a large scale. We also do minimally invasive procedures for sleep apnea in the office and we have dentists that work with us and we make oral appliances for the treatment of sleep apnea. So, comprehensive treatment for obstructive sleep apnea and evaluation of new technology, including consumer technology, such as wearables and sensors.
Brian: As someone who has sleep apnea myself, my doctors told me consistently that it’s not only a problem with being tired, but it contributes to a lot of other chronic illnesses that can be –
Dr. Stern: Absolutely. So what’s exciting for me to be here at eClinicalWorks is to meet practitioners in other specialties and being able to discuss with them the fact, as you say, undiagnosed sleep apnea contributes significantly to high blood pressure, to diabetes, to anxietyand depression, and, overall, significantly increasing the cost of healthcare for those patients that are undiagnosed. Let me give you a couple of numbers. It’s been estimated by Harvard study, and already six years ago, that the burden to the US economy of untreated sleep apnea is $160 billion, with a b, billion dollars per year. Whereas the cost of treatment would only be $10 to $12 billion.
Brian: Wow, those are some amazing numbers. So, we were talking about wearables and particularly you were mentioning wearables for, not diagnosing, but seeing the beginnings possibly of sleep apnea – can you talk a little bit about that particular device?
Dr. Stern: Yeah, so wearables have become very popular and they’ve been used primarily for the activity wearables for weight control, for exercise evaluation.
Brian: A FitBit, for example.
Dr. Stern: For example, the Fitbit is a very well-known wearable. They purport to evaluate sleep, they really evaluate movement – so they may be able to tell you when you’ve gone to bed, when you’ve woken up, but they won’t give you information about the quality of the sleep, and they won’t give you information about the likelihood of you may be suffering from sleep apnea. Now, they are not medical devices, so that’s not their role. However, there are some sleep sensors, and one of them we’ve worked with and we’ve been able to bring into healow so that the eClinical physicians can access the data, and that sensor is called Beddit. It’s not really a wearable, because you don’t wear it. It’s placed on your mattress and every time you go to bed it starts picking up data from the hours that you’re sleeping, the quality of your sleep, and it also picks up breathing – so it can tell you how well you’re breathing and if you stop breathing. It, again, is not a medical diagnostic test, but it can help raise awareness among the users, as well as the doctors. What’s very exciting is that this is the first consumer sleep sensor that’s been integrated into an Electronic Health Record system through healow. So, it makes it very easy for that data to have some meaning, because the problem with wearables and sensors is that they’re there and people look at the numbers, the question is the “So what?” So, in this case it’s “Hey, we can show this to a doctor who’s using eClinicalWorks,’”and that information can actually come in to the Electronic Health Record system and be used to raise the question that this patient may be suffering from sleep apnea. The next step would be to refer that patient to a sleep specialist. I’d like to mention something else that we’ve used with eClinicalWorks is telehealth and Telemedicine. There are not enough sleep doctors in the Unites States, there are not enough sleep centers to identify, diagnose and treat all the patients suffering from sleep apnea and other sleep disorders. So, being able to evaluate patients through telemedicine and telehealth is something that we’ve just started doing, using the eClinical system, and I think that that’ll be another great improvement to try to identify those that are suffering from sleep apnea.
Brian: That’s fantastic, because with so many different specialties, there is just such a limited number of specialists in those areas, that telehealth really does really, would be very, very helpful. To go back to the beddit, I actually had the opportunity to go to their site here at the conference, and while we were talking about how that information can be fed directly into eClinicalWorks, which is obviously a fantastic step forward – I was fascinated by what the consumer got out of it – the number of graphs, the amount of information that were provided on your phone, directly in front of you. Really fascinating stuff. It’s inspiring, and it inspires you to take action of your own health.
Dr. Stern: Yes, the sensors and the activity trackers, that’s the first thing they do. They kind of raise awareness and they get you motivated to do something. Interestingly, most people stop using them after three months. So, what’s great about this sensor and this connection to eClinicalWorks is there are continuous data that are transmitted into healow and eClinicalWorks when the owners are using these devices. Beddit is very forward thinking and they have created a sleep report that can be generated from this, and not just individual numbers but a two-week report of sleep that can be made available to the primary care doctors and to sleep doctors, as well. Not only a curiosity of your sleep but these are things you can do based on this report. One of the other things that we do at BlueSleep is we provide sleep coaching. It’s not a medical service, it’s a sleep wellness service, and it allows us throughout the United States, in fact throughout the world, to be able to advise people on better sleep, better habits, and raise the possibility that they may be suffering from a sleep disorder.
Brian: You mentioned earlier that you’ve been using wearables, if you will, for 15 years, and that you’re using telemed now, etc. So, it seems that your practices are very, very cutting edge with technology. One last question would be, where do you see this type of technology going in the future, and how do you see this affecting both providers and patients?
Dr. Stern: I would say that this year is a pivotal year, in terms of consumer technology, actually coming into the consciousness of the medical providers and through, for example, a Portal through eClinicalWorks. I had the pleasure of meeting Melissa Alexander, who did the project with us of integrating Beddit into eClinicalWorks, and I met her at a conference called Health 2.0. Health 2.0 is a digital startup group and conference, and this year they seem to all be asking the question, “We have cool technology, but now what do we do with it?” This is the first year that I heard them pose that question, and I think the answer is – let’s use that technology, let’s see how it can raise awareness, not only among the patients, but also the doctors, for example, that sleep is important, and what we can do about it? So, I think that integration of consumer technology with the Electronic Health Records system is critical. One of the other things I want to say is that when Girish and Dr. Raj talked about safety, and patient safety, at another level, at a different level, sleep impacts patient safety by improving the likelihood of diagnosis of undiagnosed diseases. So I would say that’s improving patient safety. At the same time, better sleep helps people drive safer, it decreases accidents at the workplace. Last year, there were 1,500 fatalities related to drowsy driving, 77,000 injuries, $40 billion worth of medical cost. Now, if through the trackers, we could raise awareness of how important sleep is to your health in general, that’s another area we could improve safety, and really make an impact on a very large scale.
Brian: Thank you very much for joining us here today, doctor – this was a fascinating interview and I really appreciate your time, and I’m glad that you enjoyed the conference.
Dr. Stern: My pleasure, yes. And I will be coming back.
Brian: Great, we’ll see you again next year then. Thanks for joining us. Remember, you can see more of our podcasts on iTunes, YouTube, and my.eclinicalworks.com. This is Brian Saal, have a great day.
Granting Wishes for One Child at a Time
Transcription:
Adam: Hello and welcome to this edition of the eClinicalWorks Podcast, broadcasting to you from the eClinicalWorks National Conference in Orlando, Florida 2016. I’m Adam Siladi. eClinicalWorks does a lot of work in the ambulatory space, helping physicians provide care to their patients, but they also like to give back and that’s why we’re here speaking with one of our charity partners. I have with me, Adrianne Philion, who is with ‘Give Kids the World.’ Adrianne, how are you doing today?
Adrianne: Good, wonderful. Thank you for having us.
Adam: So, tell us a little bit about your organization.
Adrianne: Yeah, Give Kids the World is a 79-acred, non-profit resort that fulfills the wishes of kids with life-threatening illnesses from across the country and around the world. The most wish, on the globe, is a wish here to Central Florida to enjoy everything that the greater city of Orlando has; from Walt Disney World, Universal, and SeaWorld. So we take that wish-child and their entire family to our resort – Give Kids the World a cost-free, week-long wish trip.
Adam: So this isn’t just a national thing, it’s an international thing and you bring kids from all over. How do they hear about Give Kids the World?
Adrianne: Yeah, so we have actually fulfilled over 150,000 wishes from all 50 states and 76 different countries. We work with wish-granters, 246 world-wide, most popularly from Make-A-Wish, Sunshine Factory, all different wish-grantors. With them, the most popular wish is a wish to Orlando, so anytime they have a wish-child who that is their desired wish, we then have to fulfill it.
Adam: I’m sure you work very closely with a lot of pediatrics practices, and other organizations that deal with children…
Adrianne: Yeah, so a lot of the time a family doesn’t know ‘Hey my child has been diagnosed with a life-threatening illness, they’re eligible for a wish.’ Usually, you know a doctor, a nurse, a social worker, a family friend, recommends them to a local wish-granting organization.
Adam: So, they make a wish, the wish is granted through one of these organizations, and then they arrive at your in Orlando, Florida, and then what happens next?
Adrianne: So, we actually greet the families at the airport, so we want to make, as soon as they touchdown here at the city, kick it off with a seamless, worry-free, perfect wish trip. So, we have volunteers that greet them at all the airports, and then help transport them back to the village. We provide them with three days to Disney, two days to Universal, and a day to SeaWorld, and any other theme park that they would like, but the big three are the ones that they’re automatically going to get, and we try to make that week as magical and full of family memories as we can.
Adam: That sounds very all-inclusive. I mean I don’t think I’ve seen anything that good on groupon, or anything like that.
Adrianne: Our guests are very special, it’s a very elite guest list that we have because all our families have a child who’s battling a serious illness.
Adam: Now you work full-time for the organization, but I’m sure there’s a lot to get done. How does all that stuff get done?
Adrianne: It really, truly takes a village to make Give Kids the World village happen. So we have a village of about 19,000 volunteers because every week we have about 1700 volunteer shifts that need to be filled. Our volunteers are the ones serving the meals in gingerbread house, they’re serving ice cream in the ice cream palace, they’re delivering gifts, daily, to our families, they’re meeting them at the airport, they’re in guest services, we could not do it without our dedicated volunteers we have here in the area, but also our volunteers that come internationally to help at the village.
Adam: So that brings me to a question, I didn’t realize that this when I was talking to you first, but Give Kids the World village, I thought we were talking about World Village, but you’re talking about Give Kids the World and then there’s village, so that’s the resort part, right?
Adrianne: Yeah, so we’re 79 acres, and we are a resort just for these wish-children and their families. It has everything they need from dining facilities, they stay in villas – they look like cottages and castles, right out of a storybook and it’s their home for a week. It has everything they need, we have free rides for them, a carousel, a train, a dumbo-type ride that they can go on, two pools, we do therapeutic hor-back riding. We also celebrate a different holiday every night of the week. So, everything Monday’s Halloween, every Thursday is Winter Wonderland – we celebrate some of those Christmas-type holidays because holidays aren’t always a guaranteed experience for our families, so we try to jam-pack a year’s worth of holidays into their one week.
Adam: Wow, and Halloween every Monday – how do you come up with that many costumes? Do you have a closet full of costumes, in rotation?
Adrianne: Yeah, in every size you could imagine, Tinkerbell and Cinderella, but also buckets and buckets and tubs full of candy every week. And if you think our kids, sometimes they’re battling some serious illnesses and they may have different dietary needs, too, so we want to accommodate all different candy because while they’re at the village, it’s their new normal so they can do anything – everything is handicapped accessible, every food, it’s for them, they can eat, they’re not limited by their disabilities, in the real world. At Give Kids the World, it’s a kid’s world and everything is limitless for them.
Adam: Do you have a favorite ride or activity?
Adrianne: I would say, my favorite activity is at our pool – so it’s zero entry, so kind of like the beach, which is great for Orlando. We’re close to the beach, but we’re kind of not right on it, so a lot of our families, it’s an experience for them, too. So it’s zero entry, so it feels kind of like the beach, but it’s really because, our children that are in wheelchairs, we have water-accessible wheelchairs, so they can transfer out of their regular wheelchair, into this kind of this steel PVC pipe wheelchair, and be able to swim along with their siblings and parents, a lot of the times for the first time.
Adam: Right, so it sounds like an experience that they’ve never even had before.
Adrianne: Yeah, I mean, there’s not a favorite because we do therapeutic horseback riding, seeing an international family who’s maybe never seen snow and they get to meet Santa and see snow here in Central Florida – it’s hard to pick just one favorite.
Adam: And then you mention the families, as well. So, I mean, obviously there’s a lot of attention being given to the grantee of the wish, the receiver of the wish, but what about the families? What’s their experience like?
Adrianne: The neat thing about a wish, wishes in general are the most magical thing, no matter what the child’s wish is – if it’s a celebrity, do I have a treehouse, do I have a laptop or computer, but the neat thing about a wish trip to Give Kids the World village is that it’s for the whole family. It’s for the sibling, it’s for the mom and dad, or other guardian because no matter who that family member in, it’s taking a toll on them having either a child or sibling with a life-threatening illness. I know, personally, as a wish sibling, it was very hard growing up with my brother who was battling brain cancer, sometimes you feel like you’re left out because your sibling and your parents are focusing on their survival, and so, at the village, we try to treat everyone equally – have that royal, special treatment for everyone because we know that the family is all going through a difficult time.
Adam: Wow, so this is very personal for you, as well. Obviously that’s probably why you got involved with something like that.
Adrianne: It is. I think my brother’s wish was 19 years ago, so quite a long time ago, but I think, since then, our family still talks about it, to this day about when we got slimed, eating pancakes every morning in the gingerbread house, going on the carousel as much as you want, I still get chills talking about it because it really was life-changing for our families. My dad and mom both say they hit a plateau, they didn’t know what to do with his treatment, he had stage four brain cancer, and they had viewed him as such a patient, focusing on his survival, but at Give Kids the World, they saw him as a kid, going to the theme parks, going on rides, and what family bonding can really do. There’s so many great medical advancements, but sometimes the greatest is just happiness and hope and how much that can help a child.
Adam: Well, we’ve done a lot of talking about what you do, and you said that you have a clip so that we can give people an idea of what it all looks like and how it all goes together.
Adrianne: Yes, it’s such a place you need to see.
Adam: Well, let’s cut to that clip right now and we’ll be right back.
(Give Kids the World Clip)
Adam: Well, that was such a great look at what you guys do, and to get that idea of the wonder that the kids might have when they walk in. And, of course, eClinicalWorks partners with other charitable foundations, as well. This year we’re partnered with the one Orlando fund, the national alliance to end homelessness and St. Jude’s Children’s Research Center, as well, and they all do wonderful work. eClinicalWorks has a lot of great programs to set up to support charities, as well. One of the cool things that they do is they have a matching gift, so if an employee makes a donation to a charitable organization, eClinicalWorks will match that, as well. This year at our conference, and actually after the past few years at our conferences, we’ve also done charity drives, as well, and this year eClinicalWorks is selling jackets, a very nice Eddie Bauer jackets, stylish gray, as well as a laptop messenger bag, both very cool, and all of the proceeds from that are going directly to our charity partners, so 100% of that money is going to go. I told our podcast team about some of the great stuff that you guys are doing, and they were all very moved, and so the entire podcast team went to the donation booth and we all bought eClinicalWorks jackets to support our charity partners and we just wanted to say that you guys are doing a great job, and our other charity partners are doing a great job. So thank you for taking the time to speak with us, and keep it up, keep up the good work. For the eClinicalWorks Podcast, I’m Adam Siladi, thanks for watching.