Supercharged Superusers on the Great Plains – Part 2
Published on Wednesday, August 30, 2017
Brown Clinic isn’t the biggest clinic in the Midwest, but don’t let size fool you. With self-trained superusers on board, this Watertown, South Dakota practice has employed the full power of eClinicalWorks to achieve PCMH recognition, take on the challenge of Chronic Care Management, and find success as a new Accountable Care Organization.
“As far as the system goes and how that’s helped us remain independent? We can do a lot with the eClinicalWorks software, things that are not as easy for some of our surrounding neighbors or competitors. We oftentimes have people come to visit and talk about gaining information to share. As far as reporting — and these are skilled nursing facilities and whatnot — when they come and see what we can do, they’re just blown away!”
– Steve Kurban, Director, Revenue Cycle & Information Management

Topics From This Episode
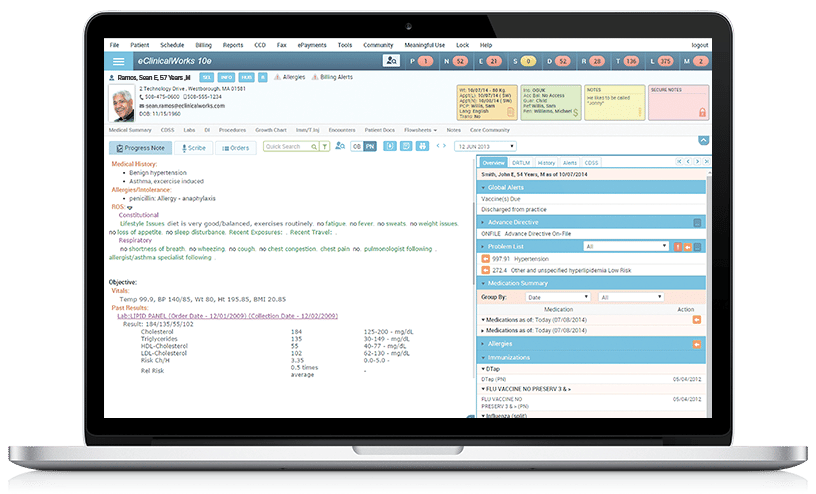
10e
The eClinicalWorks 10e EHR has transformed workflows at Brown Clinic, saving staff countless hours that used to be invested in auditing patient charts and releasing information to other providers and area hospitals. “10e has made it much easier,” says Brown Clinic data guru Steve Kurban.
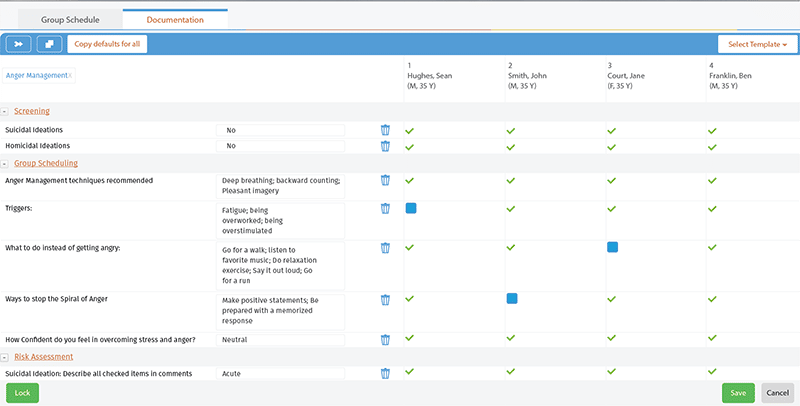
Care Planning
Even before they switched to eClinicalWorks, providers at Brown Clinic had deep experience with reporting and care planning, thanks to their participation in the South Dakota Medicaid health home program. Now, with eClinicalWorks in place, Brown Clinic is able to combine that experience and their new healthcare IT tools into effective care planning processes that are improving outcomes for thousands of patients, while helping Brown Clinic achieve its goals as a new Accountable Care Organization.
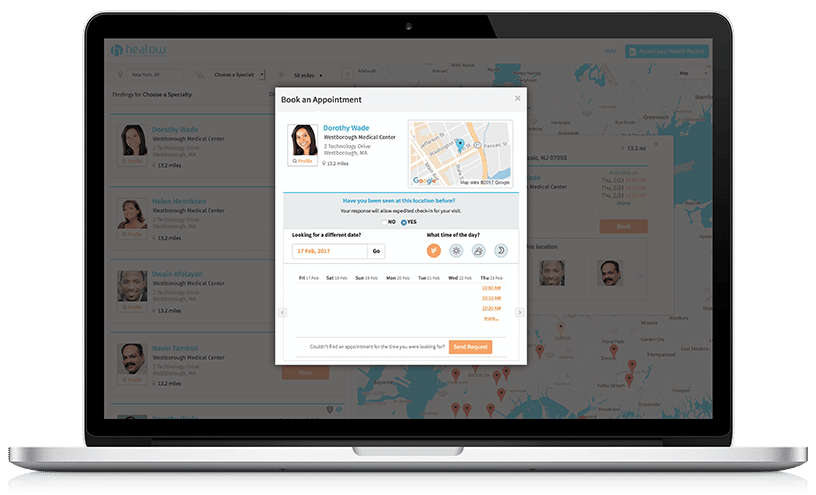
Patient Engagement tools
Want to empower your patients? Brown Clinic could literally hold a clinic on that. They’ve rolled out the healow Mom app for expectant mothers, actively use Messenger for health campaigns and reminders, and web-enable their patients in the use of Patient Portal for records access and communication.
Transcription:
Adam: One of the main focuses of healthcare today is, how do we get the most out of the healthcare system and when it comes to your EHR it’s no different. We want to learn how we can squeeze the most value out of that tool we’ve been provided, and some users take this to the next level to become “superusers.” And here to speak with us about that today are Steve Kurban and Jen Davis from Brown Clinic here in Watertown, South Dakota. Thank you guys both for being here today.
Steve: You bet.
Jen: Thanks for having us.
Steve: Before we get started with the questions that I think everyone is eager to ask, tell us a little bit about Brown Clinic. What is it all about?
Steve: Sure, Brown Clinic is one of the few independent multi-specialty practices here in South Dakota. We provide a wide range of healthcare services for the immediate community and the surrounding area. We have surgeons — a couple surgeons, an OB/GYN doctor, internal medicine, family practice, and pretty much a one-stop shop. We have our own lab and radiology department as well.
Adam: I believe you guys mentioned that you guys are also part of an ACO?
Steve: Yes, we joined a physician-led ACO, ACCO Care in Sioux Falls. We’re in our second year now.
Adam: All right, big changes there. I’m sure that’s a big adventure. So, let’s talk about that idea about a superuser. What do you think defines a superuser and how does that set them apart from other users?
Jen: What defines a superuser? Probably somebody that is generalized in knowing how the entire facility works because it’s not just, you can’t just know one little piece of how the facility works. You have to know how it’s going to interact with a different piece of the software. You also have to know a little bit about medical and a little bit about billing in order to make it all work together.
Steve: I’d say probably one of the biggest things is you have to have a person who’s willing to be open-minded enough to engage the process and learn new stuff, and help you be an advocate for your technology.
Adam: You mentioned process. I would really love to talk about that a little bit later. Let’s ask the question: You know, you’ve reached this level of superuser, you guys are both superusers here at Brown Clinic. What is your role here as a superuser?
Steve: Well, I’m the director of revenue cycle management, so I run the billing office, so I have to make sure we do the billing components the way that we do. At the same time, I kind of got a background a little bit in IT, so I try to help the technical pieces. Sometimes when you have someone who’s technical minded but not clinically minded it’s hard to bridge that gap. So I try to help work through that. Jen and I work together quite a lot on projects. As far as implementations and getting like what you started with we want to squeeze all the value we can. And to me the only way you’re going to do that is embrace it and implement it. If you have an a la carte table of tools and modules you want to maximize the use of those because certainly they’re going to complement each other and you might find a benefit down the road you don’t know.
Jen: So, I started out in a lab here so the clinical side of things and then I moved over into IT andso I do a lot of IT but I also am kind of a liaison betweenthe clinical and technical side of things as well. We work with many vendors to make the whole think work.
Steve: Especially as it relates to interfacing and stuff like that, there’s a lot of legwork that goes into that.
Adam: So, your goal is to basically push the push the adoption all of these tools you mentioned. You’re using those tools that eClinicalWorks provides.
Steve: Right.
Adam: So you guys feel that your role is to kind of drive that adoption here at brown clinic?
Steve: Pretty much, and I think if we can apply it to some value. The idea is you know if you tell people to use a system because you just told them to use it. Right. They’re not going to do that. But if you show why — we’ve talked about that before — why is it we need you to click here and put that in that box? On the back side there’s an outcome that we need. You know we went through a PCMH certification and we had to go through a process of documenting things so we could report. And then in the ACO world we have the same thing. We have to document certain things that are accomplished because we have to report them at the end of the year, and If we’re not able to do that then we’ll run into some obstacles as far as that goes.
Adam: What role has your adoption of technology and your willingness to be very proficient with it played in the ability for Brown Clinic to remain independent?
Jen: Well, the whole goal of technology is to make things easier, right? And so, to make the tools work for us so we can these programs and do these things and in a faster amount of time.
Steve: I think independence has brought — like we talked earlier — it’s brought a nimble feel to it. We can just adjust and then react to things as we need to. Governmental changes, CMS makes a change or there’s a new piece we have to a new requirement that’s been bestowed on the providers to report or what have you — we can react to that a lot quicker than a system because our governance is here. We take care of the clinic and the organization runs itself. As far as the system goes and how that’s helped us remain independent, we can do a lot with the eClinicalWorks software that some of our surrounding neighbors or competitors — not necessarily. It’s not as easy for them as it is for us. We oftentimes have people come to visit and talk about gaining information to share, as far as reporting, nursing homes, skilled nursing facilities and what not. And when they come and see what we can do they’re just blown away. And for us, those pieces of technology that we use, we almost — I don’t know if we really take them for granted — but it becomes second nature. “Oh yeah, we can do that,” and we become more like, “If we don’t know how to do it today, between us and eClinicalWorks, we’re going to figure out how to make that work.” So that’s been helpful for both of us. It’s become a win-win for both Brown Clinic and eClinicalWorks, but probably more importantly for our patients.
Adam: So, you say it sounds like a mindset. Oh yeah, we can do that no problem, yeah, and you might have to figure it out. But it’s there, and the willingness to do it.
Steve: it’s a work in progress all the time.
Jen: Right. Correct. And that’s when he usually calls me and says “I have this idea…”
Steve: and we do that a lot. And if you, if you’re not willing to think outside the box, so to speak, and adapt a process. I like to think of processes when I’m trying to improve efficiency and if you use the technology and embrace it, the efficiencies will come if you just continue to work through it. It’s always a fine-tuning process.
Adam: So, let’s talk a little bit about some of the things that you’re doing here at Brown Clinic. Care management, for example, that’s a big part of the CCM program. I know a lot of people around the country are participating in that CCM part of the program. How did you implement care plans here, and how did you do that maybe a little bit differently than what you’ve seen others do to be successful?
Steve: Well, part of it was in the beginning of chronic care management, when CMS rolled that program out, we jumped on it immediately and started figuring out a way we could accomplish that here using the tools that we had. And at the time eClinicalWorks hadn’t created or rolled out that CCM module. For us in South Dakota. There’s South Dakota Medicaid health home program that requires us as providers to report the completion of certain measures and services for that smaller population, and so we had already kind of developed a process of using our people and our tools to create a care planning module, so to speak, in that way. So, for us it was a nice jumping-off point to get to what we’re doing for health home projects for the state, and actually the state consults with us quite a bit about that. And then we have that going well, so let’s just model, use that model and then translate that into Chronic Care Management. So, it was a pretty easy move. The adoption of it has taken a little while because it’s a different mindset. Reaching out and getting ahold of a patient to come in and take care of things that are going to keep them from coming in is a little weird. But that’s the whole focus, is prevention, and getting people more wellness minded.
Adam: Right, almost like, how do I see you less?
Steve: Exactly, exactly. And that’s what I said earlier. It’s kind of an oxymoron when you think about it. We want to get a hold of you so you can come in, so you don’t have to come in again, and it’s like “OK!” But that’s where healthcare has gone, and so part of the independence thing of being nimble and being able to respond and react to that certainly helps us adjust through that. So, we jumped on Chronic Care Management almost immediately. That quickly we became a growing thing for Brown Clinic. We developed a case management approach to that. We hired a case manager, nurses, RNs, and they came in and started working with our patient population. And that’s grown to the development of a director of Patient Engagement, which has been helpful for us to continue to push that out.
Adam: What about the care plans themselves that you walk through with the patient. How did you develop those?
Steve: Pretty much we took our staff that we’re working with the Medicaid health home program here and then considered the elements that were required by CMS for Chronic Care Management, and we put together a care plan model of sorts. And that’s developed now with the help of our case managers doing the day-to-day calling and working with the patients. They’ve developed templates and in many cases templating is always a “Well, if I have a diabetic, I’ll make a template for them, and I have somebody else who has another type of condition I’ll make one for them.” What we’ve tried to do, and that they’ve done a great job of doing, is creating a template that you can have flexibility, but it’s one template. You put the template in place for the care plan visits and they can adjust depending on the chronic conditions.
Adam: So there’s 27 chronic conditions that are a part of that program, I think that’s the right number. But you don’t have 27 different templates is what you’re saying.
Steve: Right.
Adam: And of course that sounds like just that alone would be unreasonable. So you’ve combined them? You sort of combine the templates into a common?
Steve: I think you’re not going to have one that does everything, but at the same time it’s like how in the old days you used a screwdriver with your hand, and now you just have a drill, where you can drill and screw in screws with it. Well, if you develop a tool that you can use for multiple pieces or multiple functions or conditions, then that’s helpful. So, they tried to capture most of the common stuff that we see, because after a while it’s not hard to determine your population and what your group of conditions are they typically are going to be faced with.
Adam: So, with MACRA in full swing this year, you guys have decided to avoid the MIPS track by joining the ACO. How did you make that decision and how is eClinicalWorks helping you with that?
Steve: To be honest with you, the ACO decision was pretty much made by the ownership, the partnership. And they saw an opportunity, or were presented an opportunity to join the ACO from like I said earlier, it’s a physician-led ACO, it’s not connected to a health system. So there is still some independence there, but the opportunity was presented to them. They worked it out, and we looked at how our capability would be to report, because that’s the biggest piece. Its chart access, auditing and reporting. And so, when the lists come from CMS of 250 or so patients per measure, somebody is going to have to look at the charts. We’ve worked with eClinicalWorks. There’s the ACO dashboard, which is somewhat helpful, but at the same time when 10e came out, that gave us the ability to roll out some agreed-to access to our ACO staff. So, they pretty much, they get on remotely and do chart audits all day, and that’s fine. For us it was “we’re going to participate and provide the information,” and we bring a large portion of the patient population that was needed to create the ACO, which was fine. And so, it’s a small ACO. There’s basically three clinic components. We’re one of the larger, and there’s another clinic that uses another system. And so, for us, the model that we already had in place was very helpful. And then, prior to the ACO, we used eClinical Works for PQRS reporting, Meaningful Use reporting, and so we were very comfortable with mining data out of the system to meet requirements. And then at the same time doing PCHM certification brought about a process mindset to documentation and some standardization. So, all of those pieces come together nicely when it comes to rolling out to the ACO. So, it was a comfortable move for us, it’s just you know now we’re now in our second year. reporting was plenty fine. We were successful in the first year, so now we’re going to see how the second year works. We have to demonstrate some savings, but we’re confidence we’re going to do that.
Adam: I just want to go back and clarify something that you mentioned. You mentioned the 10e to provide chart access. So, in case anyone’s been living under a rock and hasn’t heard, 10e is the browser version of eClinicalWorks. Access anytime, anywhere, any device — all that stuff. So, you’re actually using that utility to provide your ACO some access to the charts that otherwise might be locked in the system.
Steve: And to be honest with you, it’s kind of like, in our way, in the days of development with Carequality and CommonWell and those types of things and Health Information Exchanges that are going, on as things develop, we don’t want to wait, and as more and more requirements are laid up on the providers to report who’s going to pay for the staffing and resources for that. Well my mindset has been, you need to deposit charts? You can audit charts all day long. We do the same thing with some of our payers. We’ve given them similar access to do chart audits. So, it makes more sense if we’re all about patient care and we’re taking care of the same population of patients, why wouldn’t we share that information? The whole tenet of sharing information across the networks like Carequality and CommonWell, it’s designed to do just that. Health Information Exchange, same thing. We’re all about sharing information to continue that quality and continuity of care.
Adam: So, with the chart access, just to finish up this thought here. The chart access, what would you have been doing? Because if you’re part of an ACO, they’re going to want to see those charts. Like you said, we’ve got those quality measures from CMS. The patient might be from clinic A or B or C or wherever. So before 10e came around what do you think you would have been doing to meet those chart audits?
Steve: Well, what we were doing in the past was we would get a list of 300, 400 patients and they need this visit, that visit or these visits on the different patients on the lists that came in, and we get those in HEDIS, and also from payers, and so we’re absorbing — When I came here four years ago we had probably a part-time person doing release of information. Now I have a full FTE plus another one to do prior authorizations and all the administration that comes with it. So, I have a person dedicated to do nothing but release information all day long. I don’t want to pay for a second one, and I have the tools because of eClinicalWork’s changes with 10e, it’s so much easier. We earlier set up an arrangement with the local hospital and gave them access to eClinicalWorks, and that was a “go over there and teach their IT staff how to load clients and software,” and all these types of things on PCs. whereas now that’s a thing of the past. It’s made it much easier and their staff like it a lot too.
Adam: And I guess you don’t have to spend your own resources and your own people’s time on those chart audits. Now that group that wants that information can do it on their own.
Transcription:
Adam: You know, we focus a lot on what the office is doing to improve their own process, but the patient of course is the whole reason the doctor’s office and medicine itself exists in the first place. So, with all the changes that you guys put into place, how are you making sure that your patients don’t get left behind?
Jen: Well, we try to get them access to the Portal. We have, you know, different campaigns. We’re actually running a campaign now for moms to engage moms, and get access to healow Mom and be able to reach our OB/GYNs easily.
Steve: Right, and then at the same time in the registration process that we have developed, just its second nature for them to try to get people to be able to be in the Portal. We began the process early, some people are slow to move in technology, and in a rural community it’s old computers, and not everybody has a computer and that’s fine. But to engage the patients and share the information is one thing we started. We publish our statements online. We’ve worked out a lot of the processes and releasing patients are now used to that. Some of the other health systems in the area also have that kind of a capability. So, we do that, it’s not foreign. But the other side is, is when we go through that and implement those things, one of the things that I try to get my staff in the business office and health information is to get them to understand just that: When the patient’s there, we have to make sure they get it. We can throw all the stuff at them we want, all the great tech, “Yeah, we can send you this and we can send you that.” And they are not seeing it. And if we can’t make that connection, it’s of no help to anybody. And so the thing is, little by little we get a report developed with our patient population that will help when it comes to navigating changes in health insurance. How do they deal with high deductibles? How are they going to manage just getting the health care they need when the costs don’t seem to go down, the health insurance premiums go up? They have health insurance but there’s a high deductible, so what are they paying for? Those types of things. So, we try to become — my goal here, at least at Brown Clinic, is to become a more of an advocate to help the patients navigate that process as opposed to the old bill collector mentality. We try to get away from that.
Adam: It is certainly unpredictable as it can be.
Steve: Right, right.
Adam: So, how do you help the patients make that more predictable?
Steve: Well, one of the things that we’ve recently been focused on is doing patient care estimation, and try to get people an estimate of what their costs, potentially their out-of-pocket costs could be. So they can plan. It’s still a work in progresses. We’re still developing that, but my goal is that the patients, when they are contemplating. You know, when we have a new mom, an expectant mom. If we can walk through with them, here’s typically what the costs are associated with the pregnancy and the delivery and those types of things. We can help them know today as opposed to “Oh, I’m happy I got my baby, and oh, I just got my bill.” You know, help them plan it. So, it’s just, you know, try to help people anticipate that by giving them the information to make decisions that they need to.
Jen: And I think the more you engage the patient, the less surprises they have, and the more comfortable they feel.
Steve: Exactly.
Adam: So, Jen, you mentioned a few minutes ago something about a campaign to let patients know about some of these tools. Tell us a little bit about what that campaign looks like and what the patients get.
Jen: Well, we are rolling out with our marketing. We actually have a marketing crew that helps us do this. But they’re rolling out, they rolled out videos with the providers, so they get that hometown feel from us. And so, they get to hear in the providers’ words what it means to them to service their community. And along with that then, we are rolling out healow Mom so that they can have access to that, and schedule appointments easily through the Portal if they have a Portal account. We’ve also tried to engage those that didn’t have a Portal account by allowing them access to email us directly, where we can then turn around and give them a Portal account.
Adam: Kind of redirect them?
Jen: Right, correct.
Adam: How do you let them all know that all this is out there?
Jen: Well, we have Facebook, and I think we have our website.
Steve: Social media. Our website is updated with some now — when you go to the website at brownclinic.org, on that homepage it’s going to pop up a video immediately with some of the providers, interviews, and comments about the OB care they provide and deliveries and what it means to them to take care of those people here at home. Because, the larger health systems — we have a hospital in town here — but the larger health systems are in some cases nearly 100 miles away. So, we try to keep it at home and work within the community. And there’s billboards in town and stuff like that. So, we do a fair marketing presence.
Adam: Multi channels.
Steve: Right, sure.
Adam: Are you using the campaign feature with eClinical Messenger at all to get any of those?
Steve: We’ve used it, but not specifically for this. But we have used it in the past, quite commonly for a flu shot campaign, those types of things. It’s helpful.
Adam: We do have a Medicare Wellness Visit campaign as well, which you might be using as an ACO. That might be something that your patients have gotten in the past. We’ve been talking about how you guys are superusers and how you’ve accumulated all of this knowledge that you’ve spread to the rest of your practice to drive the adoption. Do you think that a superuser is all about the information, the knowledge that they have, or is there like a process component to it.?
Jen: I think probably both, because you need the knowledge, but then you need to be able to be organized and set up how to run the process and how to implement it.
Steve: I agree that it’s kind of a combination. The other part that’s the intangibles, is if you have a smaller group of people that are comfortable with what you’re doing in the technology — a template, or a process, or an order, whatever the case happens to be — if somebody’s comfortable and confident, that’s going to by itself instill some confident and comfort in the people who are trying to learn it is because they’re not sure.
Adam: There’s some value there in that person who’s calm and collected. And like you said has that mentality of “Don’t worry, we’ll figure it out.” And that will be helpful as well. You mentioned you went through the PCMH process.
Steve: Yes.
Adam: What was that like? Was that valuable?
Steve: Very valuable, it was a long process. I think here it was nearly a little bit over a year process of understanding the requirements for reporting and all the different standards you have to meet for NCQA. We started out with a goal of getting PCMH certification. We attained Level 3 PCMH certification with the 2014 standards, and we lived through a change in the standard at the same time we were trying to become certified. So, it was almost like ramping it all up and starting over. But I think that wasn’t a bad thing. The process of living through that and developing procedures and policies and documentation requirements to meet PCMH certification requirements were helpful in the mindset of the organization — we have to do certain things. The ownership decided they wanted to become PCMH certified, so that was our goal. How we got there absolutely depended upon our staff, and they did a wonderful job. We went through that with eClinicalWorks — we had consultation services through PCMH certification, wonderful support there, walked us right down the path — although it took a little over a year. That then became the foundation we use now to jump off to other program requirements as they come across. That helped us establish the base for how we do ACO reporting and those types of things. Because it’s nothing new to us to have this requirement of having to report. So, it’s just instead of reporting this way, you just do it this way. You just tweak it a little bit and it works fine.
Adam: Right, if you have that foundation there, that process foundation, it’s easy to change it, and you know, as you said, I think that there’s a value there in making sure that it’s written down, making sure that everyone knows that it’s very strong.
Steve: Right, absolutely. As you move along, if you have a good foundation of a process, you can adapt it pretty much to everything. And what we do is healthcare is healthcare is healthcare. We’re still all about taking care of patients. That’s the piece you can’t lose focus on, yes we have reporting requirements; but at the same time it still boils down to how we can provide quality care for our patients?
Adam: So, what’s up next for your group?
Steve: Well, we’re in the middle of — we just actually, just recently wer connected to Carequality network so we’re trying to forge that. Some of that is causing us to reach out to facilities outside our organization to start forging some rapport and relationship. And deal with how the technology is going to come into play. The other thing that we are working with, I was mentioning earlier, at the beginning of another client here in South Dakota. We partnered up together and are going to rally up and develop a user group in South Dakota so we can help each other. I think we’ve uncovered six clients in South Dakota right now. That could represent hundreds of miles, but it’s the, you know, we actually cross time zones, which is kind of funny, but we are collecting the group. It’s in its infancy, we’re going to start working together and then I discussed with our SAM the possibility of having like a quarterly conference call or something like that with all the SAMs and all of the client representatives just to continue to work. Because we’re all running against the same challenges, be it nationally or locally. Even here in this state we have requirements that we have to meet. So if we can help each other, it all works better. Plus,eClinicalWorks benefits from having a cross-section of knowledge in this area anyways that’s willing to help anybody.
Adam: So that’s interesting, you’re going to include the eClinicalWorks side in your user group then.
Steve: Right.
Adam: From what I’ve heard so far, that’s not been the case.
Steve: We started out thinking — and I had lots of conversation with our SAM, he’s great, great support there — we discussed the initial piece, that we only have a handful of clients, let’s get the same SAM, and then we’re all on the same page. And so, I posed that, and that was like “Yeah, well you know the time zone thing,” and other things. So at the same time there potentially could be some contractual differences with the structure of the organization and the contract with eClinicalWorks and whatnot. So, as opposed to dealing with all that, we had the conversation last week actually to talk about “Well, heck, why don’t we get them all together and we’ll just get together one a quarter or whatever.” We do weekly calls with our SAM and that’s very helpful.
Jen: I think our SAM has been really great and open with us. And so, we feel comfortable with him not necessarily just you know, sugarcoating things. You know we are here to solve a problem. We don’t necessarily want to point a finger at who for what happened. We just want to solve a problem and he’s been open and honest and transparent.
Steve: I have to say that I feel strongly that our SAM, our account manager at eClinicalWorks, is truly our advocate to eClinicalWorks on our behalf, which is wonderful. And so, the fear we had in this whole endeavor was “Don’t take our SAM away.” We want him to be the guy and all that types of things. So I think it’s going to work well and, again, I said it’s just a work in progress and I think that we’re looking forward to be able to do bigger and better things across the state.
Adam: So, with all of your knowledge and experience, what would be some recommendations that you make to other clients to be more successful with their adoption of these medical record technologies?
Jen: Probably to know your system and know what you’re trying to do. Because, I’ve told other clients before, it’s like, if you ask if eClinicalWorks can do something, technically they probably can. But it’s a matter of, does it work for your facility? Is it going to work for your process?
Steve: Education is an example. The staff that come on-site to do education when you’re doing your implementation are coming to teach and train you on how the software works as it’s designed. They’re not coming to tell you how it works in your organization. And so, how you operate and how you process in your workflows and whatnot, having a good handle on that is always a good thing. And I always say, I’ve said this for years, that in industry, in manufacturing industries, if they’re going to make a change — like changing to an EMR — if they’re going to make a change in their system on their assembly line, they adapt their processes to the new equipment and the new process. In healthcare, for some reason we get stuck on how we’ve been doing it forever, and we want to make that new tool work our old way and it doesn’t work that way all the time. So, to me it’s don’t be afraid of the technology, be willing to be open minded and embrace what you can do, and look at it as a process improvement add-on, as opposed to this “Oh my gosh, I have to use this chart, that’s too many clicks.” Well let’s work through this together, that’s one of the things I think we enjoy here. We have a good enough rapport within the organization that’s we’re constantly trying to make it better. If we can remove one click and make a doctor happy, sweet. Then that phone won’t ring for a while. Then you move on to the next call. Right?
Jen: Right.
Adam: You mentioned tools a couple times, throughout the episode. And of course, an EMR is just another tool. Like a screwdriver and drills and stuff. What kind of similarity do you see there?
Steve: For us the tools, in looking at what’s available with eClinicalWorks. Anymore EMRs aren’t one size fits all like they were 10, 15 years ago. Nowadays, it’s the pick the parts that work for you. So it’s much like you walk in and you open up this toolbox, and you’ve got all these new shiny little tools in there, and it’s like, “This is going to be fun. Well, where do I start? Which tool do I pick up to begin with?” One of the things that is a tendency for new clients, I think, when they look at it is “Well, we’re just going to do the scheduling part first, then we’ll worry about the billing part,” or “We’ll do the billing part, and then we’ll do the scheduling part, and then we’ll work on care planning or whatever.” We chose to just jump in and do the whole thing. I think that helped us or required us or forced us to learn quicker. Coming from another Electronic Medical Record system to eClinicalWorks was certainly a benefit. So that the gap wasn’t as wide for us to bridge. But the other thing is, we probably, I would say, we laugh sometimes when we’re having calls with eClinicalWorks, because they’re like “You guys at Brown Clinic, you guys use almost the whole system.” If they’re a module, we pretty much have it turned on. And so, when you go to the product activation tab, there’s not many left to activate! Because each and every piece will help you. One part may help another part, and you just don’t know it until you try it. Now have we turned off things and turned them off? Sure, but you have to be willing to explore and see how it’s going to fit in your organization. If it’s not a good fit, OK. Shut it off, that’s OK. At the same time, as we develop, we can also learn. We’ve become known to you know, if we find a glitch or a bump in the system, we’re going to call and say “Hey, this isn’t working right.” Because we have that kind of rapport with eClinicalWorks. We know our SAM and we know that we can just reach out and say “This doesn’t work,” and we work it together. It should be this, this, this. And so, I think that’s important, for people to be willing to see that, but at the same time not be afraid of it. In modules or a la carte-type environment that systems are now, people get caught up with “Well, am I going to have to pay more for that?” Sure, you’re not going to get something for nothing, but at the same time, if on the back side the cost to benefit is you have a better benefit for organization or patients or both, and it’s a win/win, why wouldn’t you want to do that?
Adam: I like that, the analogy of taking a trip to the store rather than having the anxiety of maybe, you know, having a test or something like that. How do I know it all right away? You kind of pick and choose what you’re ready for and use those things. I also like you don’t always get the hammer along with the saw. But you can buy them both and they sometimes get bundled together.
Steve: Right.
Adam: Well, we greatly appreciate your expertise and your knowledge and of course you guys have become superusers through a lot of, you know, effort and work. And, of course, eClinicalWorks also has a program to help people become superusers, where you can come to eClinicalWorks itself and be trained. So, some organizations will send a representative. Did you guys do that at all? Or did you learn it all on your own? Self-made superusers!
Steve: Self-made learning and aggressive networking at the Conference.
Adam: That’s right those Conferences. We saw you there at Nashville a couple years back. It’s great to see you, I think you guys are going back again this year too so we’re looking forward to seeing you there too. So for those of our clients who don’t as confident about making themselves into superusers, as I said, eClinicalWorks does offer a program, you can send a representative or several to eClinicalWorks. We will get you trained up and help you to reach that peak that Brown Clinic here has reached. Well, thank you guys so much for all of your time and your information. It was a great pleasure to have you here. You can check out our other episodes on iTunes, YouTube and my.eclinicalworks.com. For the eClinicalWorks Podcast, I’m Adam Siladi. Thanks for watching.





