Smart Coverage Detection Equals Better Patient Care + Stronger Bottom Line
- 6 December 2023
- Blog
Waystar
This blog is presented by Waystar as part of their sponsorship of the 2023 eClinicalWorks® and healow® National Conference.

Over 14.5 million people went through open enrollment in 2022. This included new and returning consumers. While many maintained their current plan, 45% of Americans considered a change in health insurance.
One of the biggest issues during open enrollment — whether a consumer changes their policy or not — is if each person is aware of the details of their coverage. Even if they’re not making a change, an unknown shift in plan specifics can impact their coverage and finances. Providers need to consider how best to prepare for these uncertainties.
Without insight into every available policy, it’s hard to know which coverage and eligibility provisions are correct. Having a solution that makes it easy to find hidden coverage can be a difference-maker.
Improving Eligibility Awareness
Understanding eligibility requires patients to know whether they’re covered or must pay out-of-pocket for doctor visits and procedures. This puts pressure on the provider to get a definite answer. Complex processes surrounding eligibility can lead to an increase in denials, a rise in costs, and higher volumes of manual work for providers.
Between 20%-40% of presumed self-pay patients have some form of insurance coverage. When a patient mistakenly presents as self-pay, billing staff are delayed in pursuing payment from the insurance provider. Sometimes, the patient is hit with a more significant amount. This negatively impacts the provider’s bottom line and the patient experience.
Coverage detection automation can bridge this gap and make it easier for providers to identify active insurance coverage for patients. This helps the staff reduce manual work and allows patients who believe they must pay everything out-of-pocket to discover coverage they didn’t know they had.

The Benefits of Automating Coverage Detection
Knowing a patient has some coverage is good for provider cash flow as it’s easier to recover payments from third-party payers versus patients.
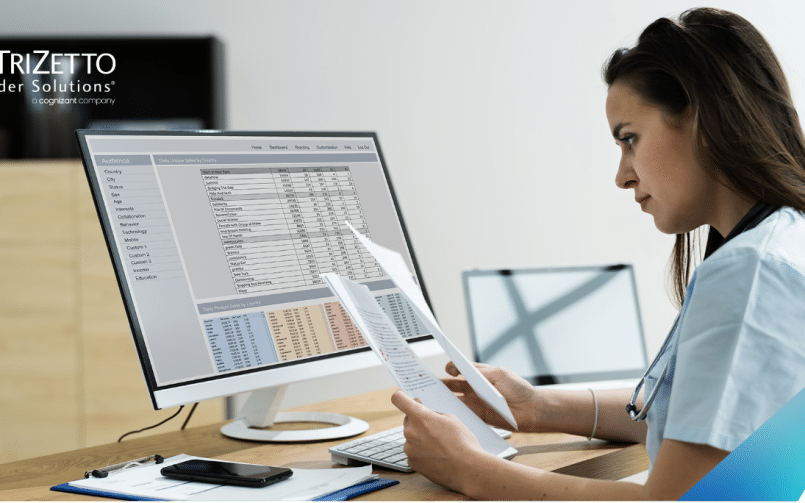
For example, providers who use Waystar Coverage Detection – which integrates with eClinicalWorks® (eCW) – can run a customized coverage detection report with specific appointment date ranges. The report makes it easy for staff to get a list of patients who identify as self-pay. From there, the software searches for active coverage and identifies patients who incorrectly presented themselves.
One Waystar client, Aultman, discovered coverage for 34% of patients who presented as self-pay, leading to a $414K boost in cash flow in just 16 months.
With Waystar’s coverage detection, providers can expect an improvement in cash flow. It also helps providers give patients better financial care. Paying out-of-pocket for medical services can be a massive hit to their finances, and having some or all of it covered by insurance provides financial relief.

What to Look for in Automated Coverage Detection
Leveraging automation should allow you to quickly confirm active coverage and find hidden coverage while simplifying and streamlining eligibility. It should also enhance coverage-related workflows for improved staff efficiency.
Active coverage automation should make it efficient to capture billable insurance that might otherwise have been overlooked. The right solution will help increase cash flow and decrease denials.
Specific features to look for include:
- Automatic coverage confirmation
- Customizable dashboards and reports
- Ability to validate patient coverage
Bringing in More Revenue While Providing Relief to Patients
Automated coverage detection allows your billing staff to offer patients a helping hand while increasing revenue. With the discovery that they have at least some insurance coverage, patients can find some financial relief from t medical expenses. Providers can get paid faster from insurance companies without investing more employee time into the process.
Discover the Way Forward with Waystar
Waystar’s revenue cycle platform combines innovative software, robust data, and unparalleled client support, streamlining workflows and improving financials so providers can focus more on patients. Trusted by 1M+ providers and 1K+ hospitals, Waystar automates $4B+ out-of-pocket estimates and claims annually for over 50% of U.S. patients. Discover the way forward at waystar.com.