Addressing the Acute Need for Chronic Care Services
- 17 August 2022
- Blog
eClinicalWorks
Employing effective tools for high-risk, high-need patients
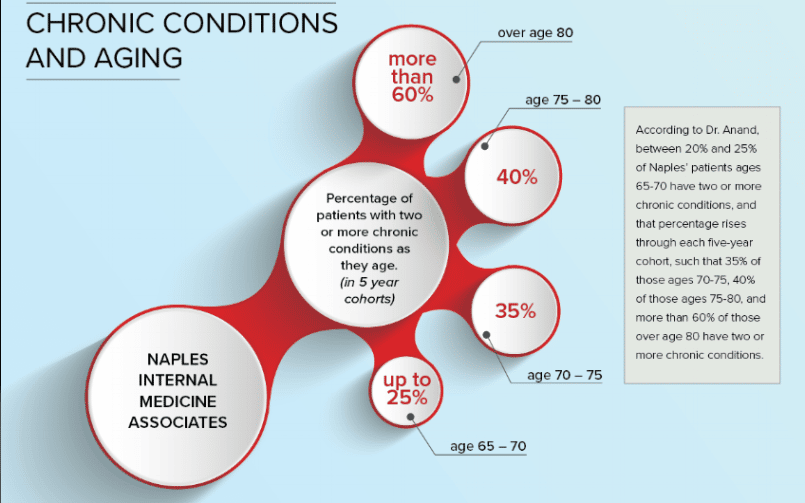
The numbers don’t lie: The older we get, the more chronic medical conditions — on average — we accumulate. Yes, there are 90-year-olds who spring out of bed and go hiking or waterskiing, but they are the exception. For most humans, age takes its inevitable toll.
As of 2018, according to this report from the Centers for Disease Control, just over half of all Americans (51.8%) have at least one chronic medical condition. And just over one-quarter of us (27.2%) have two or more such conditions.
The surprising part? Those figures are for all Americans, regardless of age. Youth may help, but it turns out to be no guarantee of good health.
Fortunately, modern medicine has the tools to fight back, helping us remain active and healthy at any age and providing medications, therapies, and rehabilitation when we need them.
The challenge of managing chronic conditions
Providers know what to do to keep their patients healthy. The real challenge is keeping track of all those appointments, lab results, prescriptions, follow-up visits, and annual screenings.
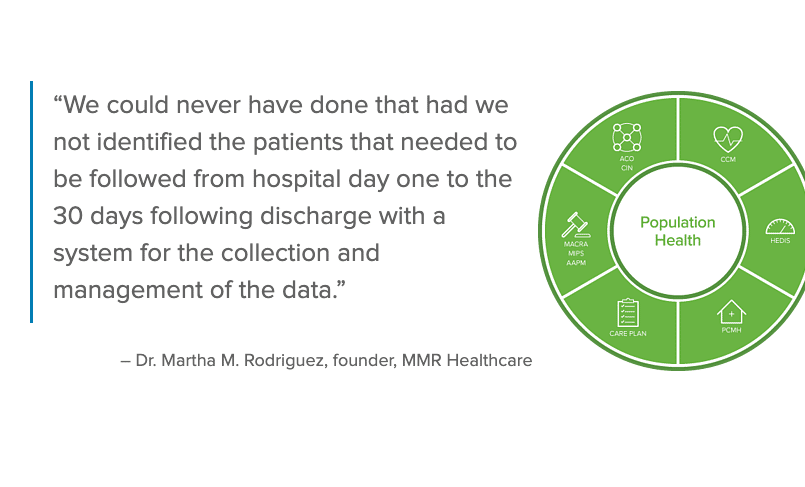
The Chronic Care Management (CCM) module from eClinicalWorks helps practices do all that and more. By helping busy providers keep track of the often complex medical needs of patients with multiple chronic conditions, it promotes better medical outcomes and higher patient satisfaction.
The CCM module helps providers:
- Identify patients who are eligible for inclusion in the CM program
- Manage enrollments and program activities
- Promote awareness of the CCM program and increase enrollment
- Choose from care plan templates for more than two dozen chronic conditions
- Use a time tracker to automatically record the time spent on patient care
- Simply claim submission with batch billing automation
Real-world success stories using CCM
Some practices and providers might look at a tool such as the CCM module and wonder why they cannot handle its many functions themselves. The answer is that many practices do exactly that and have for years. But the results are generally that they fail to capture the full revenue to which they are entitled and fall further behind over time.
The CCM module’s power lies in the use of technology to streamline processes that just cannot be done as efficiently any other way. It helps practices improve revenue flow for providing services they have always provided, while freeing staff to do more direct patient care and less paperwork.
Many eClinicalWorks practices and organizations have seen benefits from the CCM Module:
- A Rhode Island multi-specialty practice serves 50,000 patients annually, many of whom reside in assisted living facilities. They make effective use of CCM, making it easier to gather all relevant patient information in one place, saving time ahead of face-to-face appointments, and making those visits more productive.
- A South Carolina primary care practice enrolls many of its older patients in its CCM program. Nurse managers regularly and proactively reach out to those patients, building relationships that can help alert them to potentially dangerous medical conditions. As a result, the practice can offer early treatment that saves and improves lives.
- A regional medical system in Northern Ohio developed a CCM program that builds teams of care providers and case managers whose outreach efforts help take the burden off physicians. The teams regularly check with their patients and can alert primary care physicians or specialists to any emerging problems in time to avoid or minimize hospitalizations.
For more information or to schedule a demo, contact pophealthsales@eclinicalworks.com.
Next month, our Population Health blog series looks at our solution for Transition Care Management (TCM), which offers providers the tools and insight they need to provide the continuity and quality of care for patients moving between acute and ambulatory settings while meeting regulatory and compliance requirements of the Centers for Medicare and Medicaid Services.